Managing heartburn while using semaglutide has become a real concern for many people who start this medication to support weight management or improve blood sugar control. Semaglutide can be extremely effective, but that effectiveness sometimes comes with digestive discomfort that is hard to ignore. Heartburn is one of the most commonly reported issues, and it can show up even in people who never dealt with reflux before starting treatment.
Semaglutide slows stomach emptying and changes how digestion works, which means stomach acid can linger longer than usual. When acid stays in the stomach instead of moving forward through digestion, it increases the chances of irritation, pressure, and that familiar burning sensation in the chest or throat. Understanding why this happens makes it easier to respond in a way that protects digestion without giving up the benefits of the medication.
What Is Semaglutide And How Does It Work?
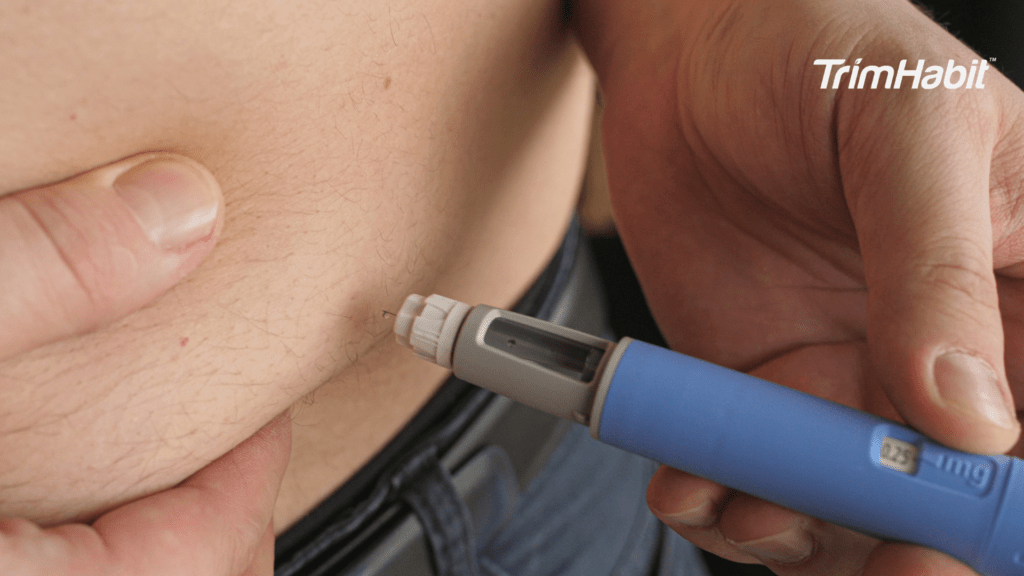
Semaglutide is a prescription medication that mimics a natural gut hormone called GLP-1 (glucagon-like peptide-1). It’s for diabetes management in people with type 2 diabetes and, at higher doses, as part of a weight loss journey for chronic weight management, helping people lose weight1.
How It Works
Semaglutide activates GLP-1 receptors throughout the body, leading to several helpful effects:
- Reduces appetite (brain): It acts on appetite centers in the brain, so you feel full sooner and less hungry.
- Slows digestion (stomach): Food leaves the stomach more slowly, which prolongs feelings of fullness and helps prevent blood sugar spikes. This process is known as delayed gastric emptying, and it can result in more acid remaining in the stomach for extended periods, which may contribute to heartburn or acid reflux.
- Improves insulin response (pancreas): It increases insulin release only when blood sugar levels are high and reduces glucagon, thereby improving glucose control.
- Lowers blood sugar overall: The combined effects help stabilize blood sugar levels in type 2 diabetes.
Common Side Effects
- Nausea
- Vomiting
- Diarrhea or constipation
- Stomach cramping
- Decreased appetite
These often improve as your body adjusts to them.
Understanding Heartburn
Heartburn is a burning discomfort felt in the chest, usually behind the breastbone. It is often described as a burning feeling in the chest or throat. Despite its name, it has nothing to do with the heart. It’s caused by stomach acid flowing back into the esophagus.
What causes heartburn?
Heartburn happens when the lower esophageal sphincter (LES), a ring of muscle that acts like a valve between the esophagus and stomach, relaxes or weakens when it shouldn’t. When this happens, acid reflux occurs when acid from the stomach flows back into the esophagus, irritating its lining.
Common Triggers
- Foods and drinks: Certain foods, especially those high in fat, can trigger reflux. These include spicy foods, fatty or fried foods, chocolate, citrus fruits, tomatoes, coffee, and alcoholic beverages.
- Large meals or eating late at night
- Lying down or bending over after eating
- Pregnancy
- Obesity
- Smoking
- Certain medications (e.g., NSAIDs, some blood pressure meds)
Limiting high-fat foods can help reduce the risk of heartburn symptoms.
Typical Symptoms
- Experiencing acid reflux, which is common among those with heartburn
- Burning sensation in the chest (often after eating)
- Sour or bitter taste in the mouth
- Regurgitation of food or liquid
- Chest discomfort that worsens when lying down or bending over
Heartburn vs. GERD
- Occasional heartburn: Common and usually harmless
- GERD (Gastroesophageal Reflux Disease): Diagnosed when reflux happens frequently (2+ times per week) or causes complications like inflammation or difficulty swallowing.
Why Semaglutide May Trigger Or Worsen Heartburn
Experiencing heartburn after starting semaglutide is a common and often temporary response. Many people notice changes in digestion as the body adjusts to the medication, even if they have never had reflux before. This reaction does not mean something is wrong or that treatment needs to stop. It reflects how semaglutide influences the digestive system, which can make certain symptoms more noticeable during use.
Slowed Stomach Emptying (Gastroparesis-like Effect)
Semaglutide intentionally slows the rate at which food leaves the stomach.
- Food and acid stay in the stomach longer
- This increases pressure inside the stomach
- Pressure makes it easier for acid to push upward into the esophagus
Result: acid reflux and heartburn
Increased Stomach Fullness
People often feel full quickly on semaglutide, even after eating small meals.
- A fuller stomach = more upward pressure
- This pressure can overcome the lower esophageal sphincter (LES)
Result: burning sensation, regurgitation
Relaxation of the Lower Esophageal Sphincter (LES)
GLP-1 medications may indirectly affect the LES, the muscle that keeps stomach acid from flowing backward.
- If the LES relaxes too often or isn’t strong enough
- Acid can move into the esophagus more easily
Result: persistent or nighttime heartburn
Dose Escalation
Heartburn is more common:
- When starting semaglutide
- When increasing the dose too quickly
Your digestive system may not have time to adjust, which can increase reflux symptoms.
Nausea and Reflux Share the Same Pathway
Semaglutide commonly causes nausea, which:
- Increases stomach acid sensitivity
- Can worsen reflux symptoms
- May lead to more frequent burping or regurgitation
Common Heartburn Symptoms To Watch For
Heartburn symptoms can range from mild and occasional to frequent and disruptive. Recognizing them early can help prevent worsening reflux or complications.
Burning Sensation in the Chest
- Feels like warmth or burning behind the breastbone
- Often occurs after eating
- May worsen when lying down or bending over
Sour or Bitter Taste in the Mouth
- Caused by acid or partially digested food backing up into the throat
- Often described as a metallic, sour, or bitter taste
Regurgitation
- Sensation of food or liquid coming back up
- May occur without nausea
- It can happen when burping
Difficulty Swallowing (Dysphagia)
- Feeling that food is stuck in the chest or throat
- May be intermittent or persistent
- Can indicate esophageal irritation or narrowing
Nighttime or Positional Symptoms
- Heartburn that worsens at night
- Symptoms increase when lying flat
- May wake you from sleep
Chronic Cough or Throat Irritation
- Ongoing cough not related to illness
- Hoarseness or sore throat
- Frequent throat clearing
Excessive Belching or Bloating
- Often linked to trapped gas
- More noticeable after meals
Managing Heartburn While Using Semaglutide
Heartburn can become part of the treatment experience for some individuals using semaglutide. Rather than viewing it as an isolated symptom, it is useful to focus on how it can be addressed and, in many cases, minimized over time.
1. Foods and drinks to limit or avoid
These commonly worsen reflux, especially when digestion is slowed by semaglutide:
- Fried or high-fat foods
- Spicy foods
- Tomato-based foods and citrus fruits
- Chocolate and mint (mint and mint-flavored products can trigger acid reflux symptoms)
- Coffee (including some decaf), alcohol
- Carbonated beverages
Tip: Even small amounts can trigger heartburn when the stomach empties more slowly.
2. Heartburn-friendly food choices
Some foods are often better tolerated and gentler on digestion, such as:
- Lean proteins (chicken, turkey, fish, eggs)
- Oatmeal, overnight oats, rice, whole grains
- Bananas, melons, apples (non-citrus fruits)
- Cooked vegetables (zucchini, carrots, green beans)
- Healthy fats such as avocado, nuts, seeds, and olive oil
- Low-fat dairy or dairy alternatives
- Ginger tea as a soothing beverage for heartburn relief
3. Portion size and meal timing tips
- Focus on eating smaller meals to reduce stomach pressure and minimize acid reflux symptoms, especially when using semaglutide.
- Try smaller, more frequent meals throughout the day instead of large portions, as this can help manage heartburn and improve digestion.
- Stop eating before you feel overly full to avoid excess pressure on your stomach.
- Finish eating 2–3 hours before bedtime to reduce nighttime reflux.
- Make dinner the lightest meal of the day.
4. Eating slowly and mindfully
- Take small bites and chew thoroughly
- Eat slowly to help prevent reflux symptoms
- Pause between bites
- Eating too quickly increases bloating and reflux
5. Avoiding lying down after meals
- Stay upright for at least 30–60 minutes after eating
- Light walking is helpful
- Avoid bending or reclining
6. Elevating the head while sleeping
- Elevate the head of the bed 6–8 inches
- Use a wedge pillow if needed
- Sleeping on your left side may reduce reflux
7. Wearing loose-fitting clothing
- Tight waistbands increase abdominal pressure
- Choose comfortable clothing, especially after meals
8. Following prescribed dosing schedules
- Take semaglutide exactly as prescribed
- Weekly injections should be on the same day each week
9. Avoiding dose increases too quickly
- Rapid dose escalation increases GI side effects
- Allow your body time to adjust before increasing
10. Antacids, H2 blockers, and Proton Pump Inhibitors
- Antacids: Fast relief for occasional symptoms. Over-the-counter antacids (e.g., Tums, Mylanta) work quickly to neutralize stomach acid, providing rapid relief from heartburn.
- H2 blockers (e.g., Pepcid AC, famotidine): Longer-lasting relief. H2 blockers, such as Pepcid AC, reduce acid production for up to 12 hours and can help prevent symptoms when taken before meals.
- Proton Pump Inhibitors (PPI): Used for frequent or persistent heartburn. PPIs reduce stomach acid more strongly and are typically taken daily rather than as needed. They are often considered when symptoms occur regularly or do not respond to antacids or H2 blockers, and they should be used with medical guidance, especially during long term treatment.
11. When OTC options are appropriate
- Mild or occasional heartburn
- Short-term symptom control during dose adjustments
12. Safety considerations while on semaglutide
- Avoid long-term daily PPIs unless advised by a provider
- Watch for worsening nausea or abdominal pain
- Report persistent symptoms rather than self-treating indefinitely
When To Talk to Your Healthcare Provider
Knowing when to talk to your healthcare provider is essential, especially if you’re experiencing heartburn while using semaglutide. While mild symptoms are common early on, more severe signs require medical attention.
Frequent Heartburn
- Symptoms occur two or more times per week
- Heartburn doesn’t improve with lifestyle changes or OTC treatments
- Symptoms continue beyond the initial dose-adjustment period
Worsening or Severe Symptoms
- Increasing chest burning or pain
- Heartburn that interferes with sleep or daily activities
- Symptoms that worsen with each dose increase
Trouble Swallowing or Food Sticking
- Sensation of food getting stuck in the chest or throat
- Painful swallowing
- These may signal esophageal irritation or narrowing
Ongoing Nausea or Vomiting
- Vomiting that does not resolve
- Inability to keep food or fluids down
- Signs of dehydration (dizziness, dark urine)
Nighttime or Positional Reflux
- Heartburn that wakes you from sleep
- Symptoms that worsen when lying down despite elevation
Warning Signs that Need Urgent Evaluation
Seek immediate medical care if you experience:
- Severe chest pain or pressure
- Pain spreading to the arm, jaw, neck, or back
- Shortness of breath, dizziness, or sweating
- Vomiting blood or black, tarry stools
- Unexplained weight loss
These symptoms may not be reflux-related and must be evaluated promptly.
What Your Healthcare Provider May Do
- Review your semaglutide dose and titration schedule
- Adjust dosing or pause escalation
- Recommend short-term reflux medication
- Evaluate for GERD or other GI conditions if needed
Key Takeaway
Heartburn is a common and generally manageable effect for people taking semaglutide. Experiencing it does not mean the medication is unsafe or ineffective. Symptoms can often be reduced through strategies such as adjusting meal timing, choosing foods that are less likely to trigger reflux, and using over-the-counter or prescription medications under the guidance of a healthcare professional. Being proactive about heartburn helps you stay comfortable, maintain consistency with treatment, and support overall digestive health while using semaglutide.