Intermittent fasting continues to gain popularity as a dietary approach embraced by many individuals seeking various health benefits such as weight loss. However, what many may tend to overlook is the crucial aspect of electrolyte imbalance.
In this article, we delve into the importance of addressing electrolyte balance during intermittent fasting to ensure a healthy and sustainable fasting journey.
What Are Electrolytes?
Electrolytes are minerals found in the body that carry electrical charges. They are vital in maintaining various bodily functions, including fluid balance, muscle contractions, nerve signaling, and regulating pH.
Electrolytes facilitate cell communication and support the body’s overall functionality1.
The essential electrolytes include sodium, potassium, calcium, magnesium, chloride, and phosphate. Each of these electrolytes contributes uniquely to bodily processes:
Sodium
Sodium ions are vital for maintaining fluid balance, nerve function, and muscle contractions. Studies have shown sodium is crucial in regulating blood pressure and cardiovascular health1,2.
Potassium
Potassium is essential for proper muscle function, nerve transmission, and fluid balance within cells1.
Research suggests that adequate potassium intake may help lower blood pressure and reduce the risk of stroke3.
Chloride
Chloride ions work alongside sodium to maintain fluid balance and regulate blood pressure.
Studies have shown chloride plays a role in acid-base balance and stomach acid production, aiding digestion4.
Magnesium
Magnesium involves hundreds of enzymatic reactions in the body, including energy production, muscle and nerve function, and bone health1.
Research suggests magnesium deficiency may contribute to various health conditions, such as cardiovascular disease and diabetes5.
Calcium
Calcium is crucial for bone health, muscle function, nerve transmission, and hormone secretion6,7.
Studies have linked adequate calcium intake to a reduced risk of osteoporosis and improved bone density8.
Phosphate
Phosphate is essential for forming bones and teeth, energy metabolism, and DNA synthesis.
Research suggests that phosphate imbalance may contribute to various health issues, including cardiovascular disease and kidney disorders9.
Electrolyte Imbalance And Intermittent Fasting
Intermittent fasting alters the body’s hormonal and metabolic state, impacting electrolyte balance. During fasting, especially prolonged ones, the body depletes its glycogen stores and switches to burning fat for fuel through ketosis10,11.
This metabolic shift can lead to increased urinary excretion of electrolytes, particularly sodium, potassium, and magnesium.
Additionally, reduced food intake during fasting may result in decreased intake of electrolyte-rich foods, further exacerbating the imbalance12.
Potential Risks Of Electrolyte Imbalance During Intermittent Fasting
Hyponatremia
Hyponatremia, a condition characterized by insufficient sodium in the bloodstream, arises when there is an imbalance between water and sodium levels. This imbalance manifests as either an excess of water or sodium deficiency in the blood.
This condition can cause symptoms such as headache, confusion, nausea, and, in severe cases, seizures or coma13.
The optimal range for sodium levels typically falls between 135 and 145 milliequivalents per liter (mEq/L). Hyponatremia occurs when the sodium level dips below 135 mEq/L14.
Hypokalemia
Potassium deficiency, also known as low potassium, occurs when the blood potassium level falls below 3.5 mmol per liter15. Potassium, a vital mineral, serves numerous functions in the body.
It is crucial in regulating muscle contractions, sustaining healthy nerve function, and maintaining fluid balance1.
Low potassium symptoms may include muscle weakness, cramps, irregular heartbeat, and fatigue. Some evidence indicates that a deficiency may affect insulin levels, potentially leading to elevated blood sugar levels and reduced availability of glucose, which serves as energy for your cells16.
Hypomagnesemia
Magnesium is one of the most abundant essential minerals within your body, primarily stored in your bones. Only a tiny fraction of magnesium circulates within your bloodstream1.
Low magnesium levels usually stem from reduced absorption of magnesium in the intestines or heightened excretion in the urine.
Hypomagnesemia is common among hospitalized individuals, often attributed to their underlying illness, specific surgical procedures, or the use of certain medications.
Deficient levels of magnesium have been associated with adverse outcomes among severely ill patients during hospitalization17.
Symptoms Of Electrolyte Imbalance To Watch Out For
While fasting, it becomes imperative to maintain proper electrolyte levels as the body undergoes shifts that can impact hydration and muscle functionality.
It’s important to note the variety of electrolyte imbalances that may arise, each potentially causing distinct symptoms depending on the specific electrolyte deficiency, its severity, individual health conditions, age, and other factors.
It’s crucial to be aware of these symptoms and seek medical attention during intermittent fasting, as electrolyte imbalances can have serious health consequences if left untreated. These symptoms may include:
Muscle Cramps and Weakness
Electrolyte imbalances and deficient potassium and magnesium levels can result in muscle cramps, weakness, and spasms3,5.
Fatigue and Exhaustion
Reduced electrolyte levels may contribute to feelings of fatigue, exhaustion, and overall weakness1.
Nausea and Vomiting
Electrolyte disturbances, especially hyponatremia, can cause gastrointestinal symptoms such as nausea, vomiting, and diarrhea13.
Dizziness and Lightheadedness
Changes in electrolyte levels, particularly sodium and potassium, can lead to dizziness, lightheadedness, and fainting2,3.
Irregular Heartbeat
Severe electrolyte imbalances may disrupt normal cardiac function, leading to palpitations, irregular heartbeat (arrhythmias), or cardiac arrest18.
Electrolyte Sources
The human body obtains electolytes from both internal production and dietary sources. To meet your daily electrolyte requirements, you’ll need:
Natural Food Sources Rich in Electrolyte
- Sodium: Natural sources of sodium include table salt, broth, and pickles, which provide essential electrolyte replenishment during fasting.
- Potassium: Bananas, sweet potatoes, and spinach are excellent sources of potassium, vital for maintaining electrolyte balance and supporting muscle and nerve function.
- Magnesium: Almonds, spinach, and avocados are nutrient-rich foods abundant in magnesium, crucial for various bodily functions, including muscle relaxation and energy production.
Electrolyte Supplements
Electrolyte supplements offer a convenient way to replenish electrolytes during fasting periods. They often contain a blend of sodium, potassium, magnesium, and other essential minerals to support hydration and overall well-being.
While electrolyte supplements can effectively prevent deficiencies, choosing high-quality supplements and following dosage recommendations is vital to avoid overconsumption.
Addressing Electrolyte Balance During Intermittent Fasting: What To Know?
Maintaining proper electrolyte balance is critical for overall health and optimal bodily functions. Electrolytes regulate hydration levels, support nerve and muscle function, help maintain pH balance, and facilitate various biochemical reactions essential for life. Here are some ways to address electrolyte imbalances during intermittent fasting:
1. Stay hydrated.
Drinking adequate fluids, including water and herbal teas, can help maintain electrolyte levels. Adding a pinch of high-quality salt, such as Himalayan salt, to water can provide some much-needed sodium.
Maintaining proper hydration levels helps replenish vital minerals during intermittent fasting. Make sure that you have enough body fluids to prevent dehydration.
Stay adequately hydrated by drinking ample water, but avoid excessive intake. Consuming excessive fluids can lead to electrolyte depletion in your system.
2. Maintain a balanced diet.
Consuming a nutrient-dense diet during eating windows can contribute to maintaining electrolyte balance.
Include foods rich in electrolytes, such as leafy greens, avocados, nuts, seeds, and seafood.
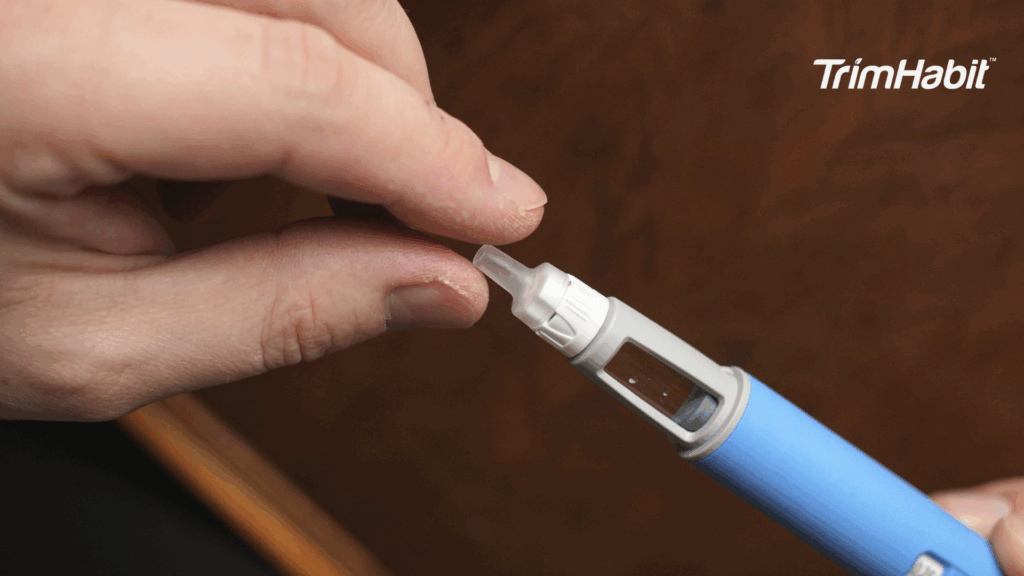
3. Consume electrolytes supplement.
In some cases, electrolyte supplementation might be beneficial in maintaining the body’s electrolyte balance, especially during extended fasting periods. There are unsweetened electrolyte supplements with essential minerals to add to your drinks or foods.
Consult a healthcare professional or registered dietitian to determine the appropriate dosage and duration.
Remember, imbalances in electrolyte levels can lead to symptoms such as muscle cramps, weakness, fatigue, irregular heartbeat, and, in severe cases, can be life-threatening.
Therefore, anyone practicing intermittent fasting should maintain electrolyte balance through diet and supplementation, essential for overall health and well-being.
Final Thoughts
Maintaining electrolyte balance during intermittent fasting is incredibly important and should not be overlooked. Electrolytes play a crucial role in various physiological processes, including hydration, nerve function, and muscle contraction, all essential for overall health and well-being.
Prioritizing electrolyte balance throughout the fasting journey is imperative to avoid potential complications such as muscle cramps, weakness, and fatigue. Maintaining optimal electrolyte levels can help sustain energy levels and support the body’s adaptation to fasting.
Critical takeaways for effectively maintaining electrolyte balance during intermittent fasting include ensuring adequate electrolyte-rich foods and beverages, incorporating electrolyte supplements when necessary, and staying hydrated.
Balancing electrolytes involves consuming various foods rich in sodium, potassium, magnesium, and other essential minerals to meet daily requirements. Additionally, paying attention to hydration levels and adjusting fluid intake accordingly can help prevent electrolyte imbalances.
Lastly, individuals embarking on intermittent fasting should prioritize their health and well-being. While intermittent fasting can offer numerous health benefits, it’s essential to adjust to your body’s signals and seeking professional advice if needed is essential.
Consulting healthcare professionals, such as dietitians or physicians, can provide personalized guidance and support to ensure safe and effective fasting practices. It’s important to remember that even with adequate electrolytes, everyone’s body responds differently to fasting; what works for one person may not be suitable for another. Always prioritize what’s best for your body, and you’ll achieve the desired outcomes.