Can intermittent fasting harm your heart? This question has sparked debate among health experts and individuals considering fasting as part of their dietary habits. While some believe it may increase cardiovascular risk, others argue that it strengthens the heart.
Let us examine the facts and clear up common misconceptions.
What Is Intermittent Fasting?
Intermittent fasting is a way of structuring your eating by alternating between periods of eating and fasting. It does not dictate specific foods but focuses on timing. Common schedules include 16:8, where you fast for 16 hours and eat within an 8-hour window, or 5:2, where you eat normally for five days and restrict calories for the other two. Some use it for weight control, better digestion, or blood sugar management, while others find it more convenient than constant meal planning.
Myths about fasting, such as the belief that skipping breakfast harms metabolism or causes heart disease, make some people question whether it is safe or effective. Let’s look at these myths and explain why they aren’t necessarily true.
Myth #1: Fasting Puts Excessive Strain on the Heart
One common belief is that fasting triggers stress responses that may harm the heart. While it is true that fasting activates pathways like cortisol release, the body also adapts by improving metabolic efficiency. Research suggests that intermittent fasting can reduce inflammation, improve insulin sensitivity, and lower oxidative stress, which are factors linked to heart disease1.
Additionally, intermittent fasting has been shown to lower resting heart rate and blood pressure, both of which contribute to a healthier cardiovascular system2. However, extreme fasting without proper nutrition can lead to electrolyte imbalances, which may pose risks for individuals with existing heart conditions. People who already have cardiovascular health concerns should consult a healthcare professional before making major dietary changes.
Myth #2: Fasting Increases the Risk of Arrhythmias
Some worry that fasting could lead to irregular heartbeats due to fluctuations in electrolytes and hydration levels. While prolonged fasting or improper hydration can contribute to these issues, controlled intermittent fasting with proper fluid intake does not inherently cause arrhythmias.
In fact, studies indicate that fasting may support autonomic balance, helping regulate heart rhythms rather than disrupt them. Some evidence also suggests that fasting can enhance parasympathetic nervous system activity, which promotes relaxation and stable heart function3,4.
Myth #3: Skipping Breakfast Harms Heart Health
Some people find it easier to skip breakfast as part of their fasting window due to the timing of certain fasting schedules. However, some assume that skipping breakfast leads to heart disease, but this idea comes from observational studies rather than direct proof.
Many breakfast skippers also have other lifestyle factors, such as poor diet, smoking, or sedentary behavior, that contribute to heart issues. Intermittent fasting, when paired with balanced nutrition, does not necessarily increase cardiovascular risk. Time-restricted eating, a common form of intermittent fasting, has been linked to improvements in cholesterol levels, triglycerides, and markers of inflammation5,6.
Breakfast skipping alone is not the issue, but what a person eats during their eating window plays a significant role in heart health. Consuming processed foods, high amounts of sugar, and unhealthy fats negates the benefits of fasting. On the other hand, prioritizing lean protein, fiber-rich foods, and heart-healthy fats can help maintain cardiovascular function.
Myth #4: Fasting Causes Muscle Loss, Weakening the Heart
There is a misconception that fasting leads to muscle breakdown, which could include cardiac muscle. While prolonged starvation does result in muscle loss, intermittent fasting does not cause significant muscle degradation when adequate protein intake is maintained. On the contrary, stimulates autophagy, a process that helps clear damaged cells and supports cellular repair, including in heart tissue7.
Additionally, concerns about lean muscle mass loss during intermittent fasting are often overstated. When people consume enough protein during their eating windows, they can maintain muscle while still benefiting from fasting. Proper dietary habits, including strength training and protein-rich meals, can help preserve lean muscle mass and prevent unwanted side effects.
The Impact Of Intermittent Fasting On Cholesterol And Blood Pressure
Intermittent fasting can lead to healthier cholesterol levels by lowering LDL cholesterol, which contributes to artery-clogging plaque, and increasing HDL cholesterol, which helps protect against heart disease. It may also enhance the function of blood vessels, improving circulation and reducing strain on the heart.
Blood pressure regulation is another key benefit. Elevated blood pressure strains the cardiovascular system over time, raising the risk of heart failure and stroke. Intermittent fasting has been linked to reductions in systolic and diastolic blood pressure, particularly in individuals with obesity or metabolic syndrome8. This may be due to improved insulin sensitivity and reduced inflammation, both of which contribute to better vascular function.
Can Fasting Help Prevent Heart Disease?
Intermittent fasting can help the body switch more efficiently between using glucose and fat for energy, which may lower the chances of developing insulin resistance. Since insulin resistance is linked to type 2 diabetes and a higher risk of cardiovascular disease, better metabolic flexibility could support heart health.
Intermittent fasting may also play a role in reducing chronic inflammation, which is a known contributor to heart disease. In allowing the body periods of rest from digestion, fasting promotes cellular repair and reduces oxidative stress, which can contribute to arterial damage.
In addition, intermittent fasting may help reduce C-reactive protein levels, a marker of inflammation associated with heart disease. Less inflammation in the body can lower the risk of atherosclerosis, a condition where plaque builds up in the arteries, increasing the chances of heart attacks and strokes.
The Risk Factors: Who Should Be Cautious?
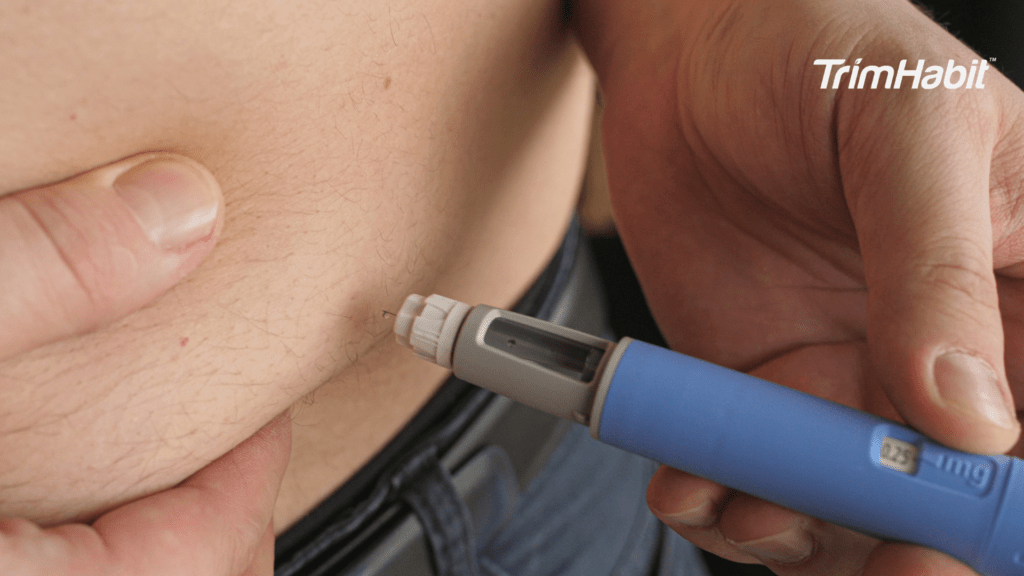
While intermittent fasting has potential heart health benefits, it is not suitable for everyone. Individuals with pre-existing heart conditions, diabetes, or a history of eating disorders should consult a healthcare professional before adopting a fasting regimen. Severe calorie restriction or extreme fasting methods can lead to nutrient deficiencies, electrolyte imbalances, and increased stress on the heart in vulnerable individuals.
Additionally, fasting may not be ideal for those taking medications that require food for proper absorption. People with eating disorders, such as anorexia or binge eating disorder, may also find that fasting worsens unhealthy behaviors and negatively impacts their physical and mental health.
People who engage in prolonged fasting without proper refeeding may also experience decreased blood sugar levels, leading to dizziness, fatigue, or fainting. Those on medications for blood pressure or diabetes should be particularly careful, as fasting can amplify the effects of these drugs. More research is needed to determine how different fasting patterns affect various populations, especially those with existing health conditions.
How To Fast Safely For Heart Health
For individuals interested in intermittent fasting while keeping heart health in mind, here are some guidelines to follow:
Hydration is Key
Hydration is essential. Drinking plenty of water throughout the fasting period helps maintain fluid balance. Herbal teas and electrolyte-rich beverages can help prevent dehydration.
Prioritize Nutrient Dense Foods
Eating nutrient-dense foods during eating windows is necessary for maintaining cardiovascular health. Whole foods rich in lean protein, healthy fats, and fiber should be prioritized. Heart-healthy foods like nuts, fish, avocados, and leafy greens provide essential nutrients that support cardiovascular function.
Avoid Processed Foods
Avoiding processed foods is just as important as selecting nutritious ones. A diet high in refined sugars, trans fats, and highly processed snacks can increase inflammation and cholesterol levels. Whole grains, fresh produce, and unprocessed protein sources are better choices.
Do Not Overdo It
Extended fasting beyond twenty-four hours should be done cautiously. It is advisable to start with shorter fasting windows and gradually adjust based on individual responses. Extreme calorie restriction for extended periods can have negative effects, especially on individuals with existing cardiovascular concerns.
Pay Attention to Your Body
Listening to the body’s signals is important. If dizziness, heart palpitations, or extreme fatigue occur, adjusting the fasting schedule or seeking medical advice is necessary. Fasting should not cause undue stress or interfere with daily functioning.
Key Takeaway: Can Intermittent Fasting Harm Your Heart?
Intermittent fasting, when done correctly, is not inherently harmful to heart health. Instead, it has been associated with reduced inflammation, better cholesterol levels, and improved metabolic function. However, balance is key. Extreme fasting or poor dietary choices can have negative effects. As with any dietary pattern, ensuring proper nutrition and hydration is essential for long term health.
For those looking to lose weight while maintaining cardiovascular health should approach intermittent fasting with a well-structured plan. It is important to avoid drastic caloric restriction, which could lead to increased risk of nutrient deficiencies. Maintaining a diet that supports heart health and lean muscle mass will allow fasting to be a beneficial rather than harmful practice.