Starting semaglutide can feel like stepping into the unknown. You might expect your appetite to change or notice some mild stomach discomfort, but feeling drained often comes out of nowhere. This is not the kind of tiredness you get after a long day. It can feel heavy, like every movement requires more effort than usual.
Some people notice it the same day they inject, while others wake up the next morning already feeling off. Even simple tasks can feel like they take extra energy, and motivation can drop without any clear reason.
That first wave of fatigue often leads to one question: is it normal to feel tired after a semaglutide injection?
For most people, the answer is yes, but the experience is more layered than a simple yes or no. The tiredness is real, and it is not imagined. Several systems in your body are adjusting at the same time.
Hormones, digestion, sleep, and the way your body handles energy are all shifting. When all of these change together, it can feel disorienting before things settle. Your body is simply finding a new balance. Recognizing that this is a temporary stage often takes the pressure off and makes the fatigue easier to manage.
How Semaglutide Interacts With The Body
Semaglutide works through a natural hormone system that influences hunger, digestion, insulin release, and glucose use. This natural hormone signals fullness to the brain, slows digestion, and alters how the body handles incoming fuel. These effects support weight management and blood sugar regulation, but they also require the body to recalibrate several internal systems at the same time1,2.
When people ask whether semaglutide make you tired, they are noticing a real physiological response. The medication changes how your body processes food and how quickly energy becomes available. That transition phase can temporarily lower energy levels until the system stabilizes.
Why Energy Can Dip During Metabolic Adjustment
Energy levels depend on how efficiently the body converts food into usable fuel. Semaglutide changes appetite and digestion, which changes how energy enters the system. When intake drops suddenly, the body shifts into conservation mode. This response is protective rather than harmful. The body simply tries to match output with input.
Energy is stored in several forms, including glycogen and fat tissue. The body stores energy to protect against scarcity, and semaglutide alters how quickly those reserves are accessed. When food intake shifts quickly, the body needs time to catch up, and fatigue can appear during that period. This fatigue is not weakness. It reflects recalibration. Once the body understands the new pattern, efficiency improves and energy often rebounds.
Factors That Contribute
1. Blood Sugar Changes And Their Impact On Fatigue
Blood sugar plays a central role in alertness, focus, and stamina. Semaglutide improves blood sugar control, which is valuable for managing diabetes and metabolic health3. However, improved control does not mean static levels. Blood sugar changes occur as insulin sensitivity improves and digestion slows. During this phase, blood glucose levels may run lower than the body is accustomed to.
Blood sugar level fluctuations can cause symptoms even when numbers remain within acceptable ranges. Mild drops can lead to shakiness, fogginess, or sudden weakness. Low blood sugar does not always mean a medical emergency, but it does affect how you feel. This is especially noticeable when meals are delayed or portions are smaller than usual. People using other glucose lowering medications may notice these effects more strongly.
2. Appetite Suppression And Reduced Intake
Semaglutide reduces appetite in a powerful and often surprising way. Many people find that hunger cues fade quickly and meals become smaller without conscious effort. Reduced food intake often leads to reduced calorie intake without intentional planning. This can create a calorie deficit that is larger than expected. When the body senses fewer calories, it conserves energy.
Reduced caloric intake semaglutide effects are common during the early phase of use. Eating less supports weight loss, but eating too little slows energy production. The body does not distinguish between intentional restriction and accidental underfueling. Fatigue becomes a signal rather than a problem. Listening to that signal allows for correction before exhaustion becomes persistent.
3. The First Few Weeks May Feel Heavier
The first few weeks on semaglutide often feel unpredictable. Digestion slows, appetite shifts, and internal timing changes. This period is widely recognized as an adjustment period. During this time, fatigue appears more often than later on. The body is learning a new metabolic language.
During the early stages, it is common to feel tired even with adequate rest. The body adjusts gradually as hormone signaling stabilizes. Energy improves as routines form and intake becomes consistent. Temporary fatigue during this stage does not predict long term outcomes. Many people report increased stability and more energy after this phase passes.
4. Sleep Disruption As A Hidden Contributor
Sleep patterns often change after starting semaglutide. Some people report difficulty falling asleep, while others wake more frequently. Disrupted sleep can occur due to mild nausea, changes in digestion, or altered meal timing. Even subtle sleep changes can lead to noticeable daytime fatigue. Poor rest amplifies any metabolic fatigue already present.
Sleep hygiene becomes especially important during semaglutide treatment. A consistent sleep schedule supports hormonal balance and glucose stability. Relaxation techniques before bed can calm the nervous system. A calming bedtime routine helps signal the body that it is safe to rest. Quality sleep supports recovery and reduces daytime fatigue significantly.
5. Nutrition Quality Matters As Much As Quantity
Food choices strongly influence energy stability. Nutrient-dense meals help maintain steady fuel availability throughout the day. Lean proteins support muscle maintenance and satiety. Healthy fats slow digestion and stabilize glucose release. Whole grains provide gradual energy rather than quick spikes.
Nutrient-dense foods also supply vitamins and minerals essential for cellular energy production. Balanced meals help prevent energy crashes linked to blood sugar changes. Frequent meals, even when small, can help maintain steadier energy. Eating intentionally matters more when appetite is reduced. These strategies help provide sustained energy without overconsumption.
6. Hydration And Its Underestimated Role
Hydration is often overlooked when fatigue appears. Semaglutide can reduce thirst cues along with hunger. This can lead to drinking less water than usual, simply because thirst cues are not as noticeable. Dehydration contributes to headaches, dizziness, and feeling drained. Many people underestimate how much this affects energy.
Staying hydrated supports circulation, digestion, and glucose transport. It also reduces strain on the kidneys and nervous system. Making hydration intentional rather than reactive helps prevent fatigue. Paying attention to hydration matters even more when you are eating less or dealing with stomach issues. Small, regular sips throughout the day are often more effective than large amounts at once.
7. Movement That Supports Rather Than Drains
Movement influences energy in complex ways. Light physical activity supports circulation and glucose use without exhausting the body. Gentle walking, stretching, or mobility work often improves alertness. This type of movement encourages oxygen delivery and metabolic balance. It also supports mood and mental clarity.
Heavy exercise during early adjustment may worsen fatigue. Listening to the body helps determine appropriate intensity. Light physical activity often reduces fatigue rather than increasing it. Over time, stamina improves as the body adapts. Movement starts to support your energy instead of wearing you down.
8. Emotional And Mental Components Of Fatigue
Fatigue is not always purely physical. Hormonal shifts influence mood and emotional regulation. Mood swings can occur during dosage changes or periods of reduced intake. Emotional fatigue often feels like physical exhaustion. Stress amplifies tiredness even when sleep and nutrition are adequate.
Feeling tired does not always mean the body lacks fuel. Sometimes the nervous system needs reassurance and rest. Managing stress supports energy stability. Calm routines and realistic expectations reduce emotional strain. Addressing mental fatigue helps physical energy recover more quickly.
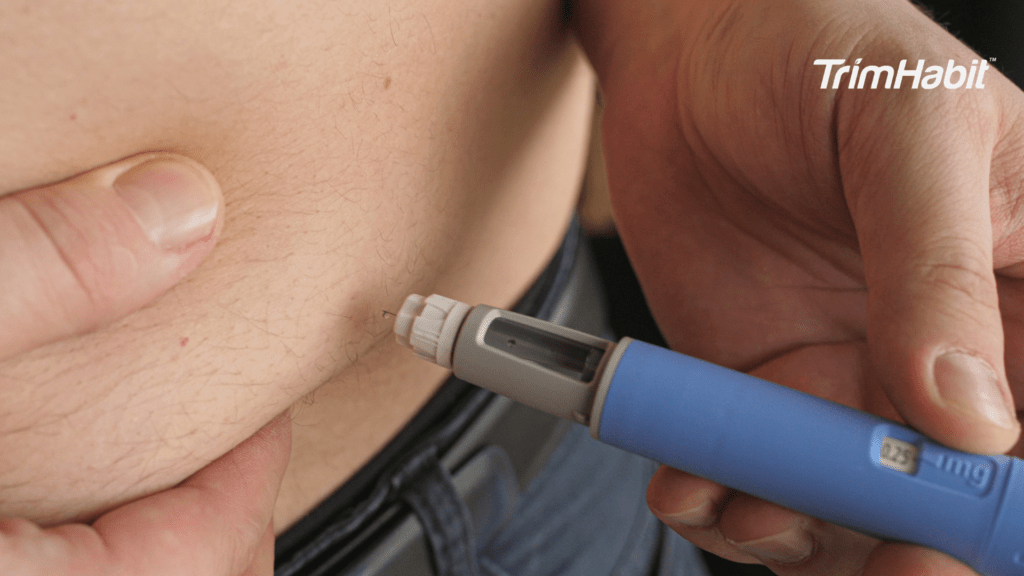
9. Injection Related Factors And Short Term Effects
Injection site reactions can occur, including mild soreness or inflammation. These reactions require immune response, which uses energy. This can contribute to temporary fatigue following an injection. Gastrointestinal symptoms such as nausea or constipation may also affect intake and sleep. These symptoms compound tiredness when not addressed.
These effects are typically mild and resolve as the body adapts. Monitoring patterns helps identify triggers. Supportive care reduces impact. Most people find these reactions lessen over time. Awareness prevents unnecessary concern.
When Fatigue Lasts Longer Than Expected
Semaglutide-related fatigue that continues beyond the initial phase deserves attention. Fatigue persists when nutrition, sleep, hydration, or medication interactions need adjustment. Daytime fatigue that interferes with work, safety, or focus should not be ignored. Persistent symptoms may require dosage review.
People using other glucose-lowering medications may need closer monitoring. Blood sugar regulation becomes more complex with multiple agents. A healthcare provider can evaluate contributing factors and adjust treatment plans. Personalized treatment plans support both progress and quality of life. Seeking guidance is proactive, not a setback.
Conclusion: Is It Normal To Feel Tired After A Semaglutide Injection?
Feeling tired after a semaglutide injection is a common and understandable side effect. Temporary fatigue reflects adaptation, not failure. The body adjusts to new signals, intake patterns, and metabolic demands. Supporting that process reduces discomfort and builds resilience.
Listening to your body matters. Responding with nourishment, rest, and patience supports recovery. If symptoms persist, guidance helps refine the treatment plan. Semaglutide supports a long-term health journey when paired with care and awareness.
Fatigue does not define the outcome. Adaptation does.