You probably expected a few changes when you first started taking semaglutide. Maybe you were ready for a smaller appetite, some early nausea, or the possibility of shifting your eating patterns. But what often surprises people most is how quickly a sense of fullness can arrive.
Imagine sitting down with a plate that looks smaller than what you used to eat. Halfway through the meal, your stomach feels heavy, your energy drops, and you wonder if you even need another bite. Instead of finishing with satisfaction, you push the plate away with discomfort.
That sensation of being overly full is not rare. Many people report that fullness sneaks up after meals, lingers long after they finish, or makes them hesitant to eat at all. While fullness might sound like a convenient side effect, in reality it can disrupt your diet, keep you from enjoying food, and sometimes interfere with your daily routine. It might even feel discouraging when you’re trying to balance your treatment plan, your weight loss goals, and your comfort.
If you’re wondering what to do if semaglutide makes you feel too full, the good news is that there are ways to manage it. Knowing why this happens, how to adjust your habits, and when to talk to a healthcare provider can help you stay on track with your medication while protecting your quality of life.
Why Does Semaglutide Cause Fullness?
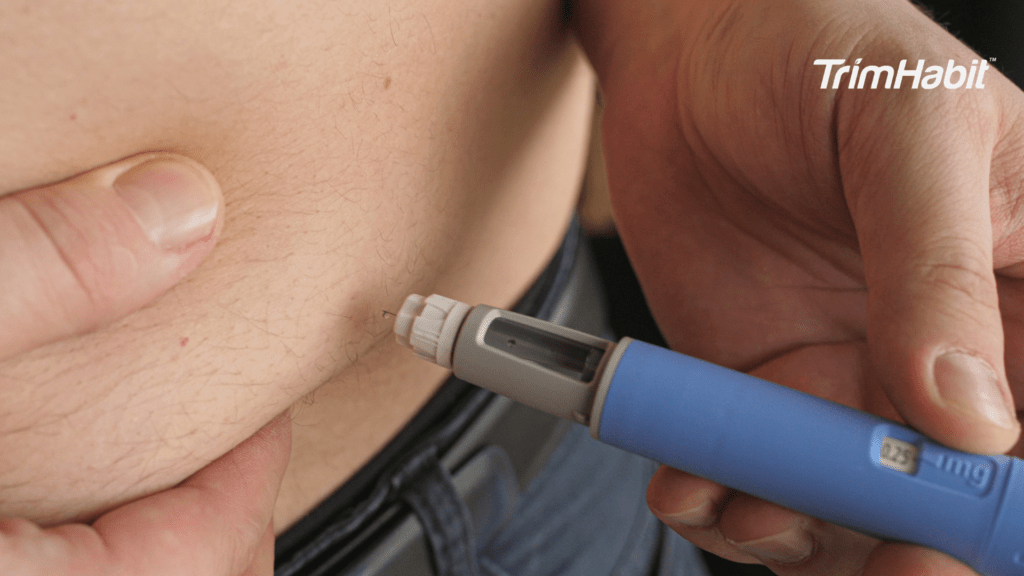
To understand the sensation, it helps to know how semaglutide works. The active ingredient belongs to a group of drugs called glucagon like peptide 1 receptor agonists. If you break down that term, it simply means the medication mimics a natural hormone your body already produces, called GLP-1. This hormone plays an important role in regulating your appetite, influencing insulin, and managing digestion1.
One of the biggest ways semaglutide involves your digestion is by slowing it down. Normally, your stomach empties food into the small intestine at a steady pace. When you begin taking medication in this class, semaglutide slows that process of gastric emptying. This delay means the food movement from your stomach into your intestines takes longer than usual.
That slower pace gives your body more time to absorb nutrients and regulate blood sugar. It also makes you feel hungry less often. For people with type 2 diabetes, this helps balance glucose control. For those with obesity, it reduces the drive to overeat and makes it easier to lose weight. These are the therapeutic benefits of the drug.
But the same mechanism that helps you with weight management can also lead to unwanted effects. When digestion drags, food lingers, and fullness builds. You may notice symptoms like bloating, heaviness, or even pressure after relatively small meals. For some, this is tolerable. For others, it becomes a daily challenge.
What Do Clinical Studies Show?
You might wonder if fullness is just your experience or a common reaction. The evidence is clear: research confirms that many people encounter this side effect.
In placebo controlled studies, participants on semaglutide consistently reported more fullness than those on placebo2. In a double-blind study of adults with obesity, once-daily oral semaglutide reduced energy intake, body weight, hunger, and food cravings while increasing fullness and satiety, without evidence of delayed gastric emptying3.
These findings show that the effect is not random, but a direct result of how the active ingredient acts on the glucagon like peptide 1 receptor agonist pathway. By slowing gastric emptying and altering appetite signals, semaglutide changes how much you want to eat and how quickly you feel full.
How Does Delayed Digestion Change Your Eating Habits?
You may have noticed that semaglutide side effects show up most clearly at the table. Meals you once considered modest may now feel overwhelming. A simple breakfast sandwich or bowl of cereal might leave you pushing away the plate. Even snacks can create discomfort if they are heavy.
This shift is directly tied to the way your body processes food. With delayed emptying, your stomach acid spends longer breaking down what you eat. That prolonged exposure can cause burning, reflux, or stomach pain. Because your food stays in place, bloating and gas also become more common.
The result is a noticeable change in your food intake. Your calorie intake may drop without you even trying. While this can seem positive for weight reduction, it can backfire if you are not getting enough nutrients. Some people find themselves skipping meals entirely because they do not want to feel sick. Others discover they no longer feel hungry in the way they used to, which makes it hard to follow a consistent diet.
Over time, this pattern can affect your sugar control. If you have diabetes, inconsistent eating might cause swings in your glucose. Even if you are not diabetic, you may feel sluggish or lightheaded when you are not fueling your body regularly. This is why managing fullness is about more than comfort. It is about protecting your overall health.
What To Do If Semaglutide Makes You Feel Too Full?
1. Shift to eating smaller portions more often
Instead of three large meals, try spreading your food into four or five lighter meals throughout the day. This prevents your stomach from becoming overly stretched at one time, which is especially important since semaglutide slows gastric emptying and makes food linger longer. By adjusting to smaller portions, you will reduce pressure on your stomach and lessen the chances of nausea, bloating, or pain.
2. Choose lighter, nutrient-dense foods
Foods high in fiber and nutrients, like leafy greens, lean proteins, and whole grains, give your body steady energy without overwhelming your digestive system. Avoid very heavy or greasy meals, which are harder to digest and more likely to cause discomfort when your stomach is already working slowly. Think about a meal of grilled chicken with roasted vegetables compared to a cheeseburger and fries — the lighter option will be easier to tolerate.
3. Drink fluids in small sips instead of large gulps
Liquids can fill your stomach quickly if you drink too much at once. Try carrying a bottle and sipping regularly throughout the day. This helps you stay hydrated, which is essential for digestion, but also avoids the “sloshy” feeling that can make you feel sick. Cold, carbonated, or very sweet drinks can sometimes worsen bloating, so stick to water, herbal teas, or clear broths.
4. Move your body after meals
Gentle movement such as walking, stretching, or light household tasks can encourage food movement through your digestive system. You do not need to do intense workouts right after eating because that may make things worse. Instead, focus on light physical activity that supports digestion, while also making it a habit to exercise regularly throughout the week. These practices help relieve gas, reduce bloating, and make you feel less heavy after meals.
5. Limit heavy or processed foods that slow digestion
Certain foods, especially those high in fat, sugar, or additives, can worsen fullness because they take longer to break down. Fried foods, rich desserts, and processed snacks often sit in your stomach for hours. While taking semaglutide, it may be best to avoid these foods or eat them only occasionally in small amounts. Replacing them with fresh produce, whole grains, and lean proteins will not only ease fullness but also support weight management.
6. Be mindful with alcohol
Drinking alcohol can irritate your stomach, interfere with digestion, and add empty calories. If you feel too full while taking semaglutide, cutting back on alcohol can help. Even small amounts can make symptoms worse, especially when combined with heavier meals. If you do choose to drink, keep it minimal and pair it with food to reduce irritation.
7. Give your body time to adjust
For many people, the sensation of being too full lessens as the body adapts to once weekly semaglutide. The first few weeks are often the hardest, but over time, your digestive system tends to balance out. Try to be patient and track your symptoms. Sometimes your healthcare provider may suggest a lower dose to help you gradually increase without overwhelming your body.
What Symptoms Should You Watch For?
Feeling too full is not always dangerous, but it can be a signal to pay closer attention. If fullness is paired with other gastrointestinal side effects, it may require closer monitoring.
Some common issues include:
- Nausea that lingers even after you stop eating.
- Constipation caused by slowed digestion.
- Vomiting if your body cannot tolerate the food volume.
- Intense bloating or the need to relieve gas constantly.
- Persistent pain in your upper abdomen or lower chest from excess stomach acid.
These problems are part of the effects of semaglutide, especially during the early stages or after a dose increase. They can be frustrating, but for most people, they improve with time as the body adapts.
However, if your symptoms grow worse or interfere with daily life, you need to consider whether the problem has moved beyond ordinary side effects.
When Should You Get Help?
There are two levels of concern when it comes to fullness. Mild discomfort is something you can often manage at home. But there are times when you should not wait.
If you experience sharp stomach pain, repeated vomiting, or cannot keep fluids down, it is time to seek immediate medical attention. Prolonged inability to eat or drink can put your overall health at risk. Similarly, if you notice that fullness and semaglutide side effects are making it impossible to stick to your treatment plan, you should reach out.
Your healthcare provider may recommend a lower dose or slower titration. Sometimes, the key is to gradually increase your medication so your system has time to adapt. A healthcare professional might also suggest diet changes, lifestyle support, or testing to rule out complications.
It is important not to wait until discomfort becomes unbearable. Getting medical attention early ensures you can continue treatment without damaging your quality of life.
Final Thoughts
Constant fullness from semaglutide can feel frustrating, but it does not mean you have to give up on your treatment or live with discomfort. By eating smaller meals, drinking water in small sips, focusing on a balanced diet, limiting drinking alcohol, and adding regular physical activity, you can manage fullness while still enjoying the benefits of medication.
If your symptoms grow severe, do not hesitate to seek immediate medical attention. Staying in touch with your healthcare provider ensures you can continue safely. With patience, lifestyle changes, and professional guidance, you can minimize semaglutide side effects and stay on the path to better overall health.