Semaglutide was originally developed to manage type 2 diabetes, but it has gained a lot of attention for helping with weight loss. While the medication can be effective on its own, the results also depend on the lifestyle habits that go along with it, especially your diet. Some high-fat or heavy foods can reduce its benefits or trigger side effects like nausea, bloating, and heartburn.
In this article, we’ll look at what not to eat when taking semaglutide and share a practical eating plan designed to support your progress while keeping discomfort to a minimum.
Semaglutide Overview
Semaglutide is a GLP-1 receptor agonist (glucagon-like peptide-1), a class of drugs that mimic the action of a natural hormone involved in blood sugar regulation and appetite control. It is sold under brands such as Ozempic, Wegovy, and Rybelsus1.
Medical Uses
Type 2 Diabetes (Ozempic, Rybelsus)
Semaglutide helps lower blood sugar levels by:
- Stimulating insulin secretion
- Suppressing glucagon (a hormone that raises blood sugar)
- Slowing gastric emptying (which reduces post-meal blood sugar spikes)
Chronic Weight Management (Wegovy)
Approved for adults with obesity or overweight with at least one weight-related condition (e.g., high blood pressure, type 2 diabetes, or high cholesterol). It reduces appetite and food intake.
Forms & Dosage
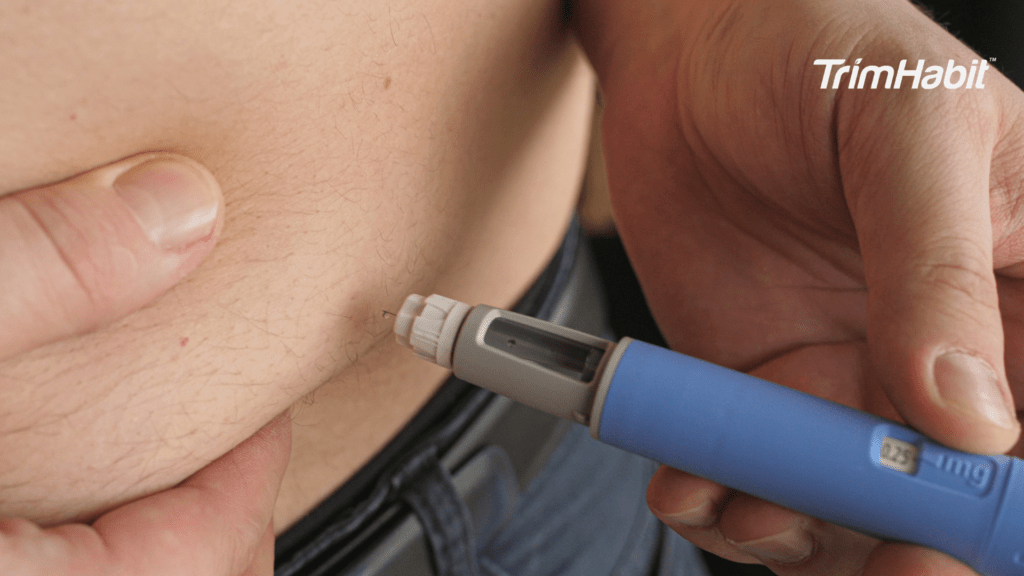
- Injectable (Ozempic, Wegovy): Weekly subcutaneous injections
- Oral (Rybelsus): Daily tablets, taken on an empty stomach
Dosages vary based on indication and patient response. The medication is typically started at a low dose and increased gradually to minimize side effects.
Benefits
- Improved blood sugar control
- Significant weight loss
- Potential cardiovascular benefits (e.g., reduced risk of heart attack and stroke in high-risk patients)
Side Effects
Common side effects include:
- Nausea
- Vomiting
- Diarrhea or constipation
- Decreased appetite
Less common but serious risks:
- Pancreatitis
- Gallbladder problems
Precautions
- Not for use in people with type 1 diabetes or diabetic ketoacidosis
- Not recommended during pregnancy or breastfeeding
- Caution in individuals with a personal/family history of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia syndrome type 2 (MEN 2)
Lifestyle Role
Semaglutide is most effective when combined with:
- Healthy eating habits
- Regular physical activity
- Behavioral changes
Why Diet Matters With Semaglutide
Semaglutide can be effective on its own, but what you eat can make a big difference. Certain foods may work against its benefits or make side effects worse.
1. Enhances Weight Loss & Blood Sugar Control
Semaglutide reduces appetite and slows stomach emptying, but your food choices can complement or counteract those effects, especially regarding blood glucose levels .
- Nutrient-dense, lower-calorie foods help promote sustainable weight loss.
- Low-glycemic foods prevent sharp blood sugar spikes, supporting better glucose control.
2. Reduces Side Effects
The most common side effects of semaglutide are nausea, bloating, and gastrointestinal discomfort. Diet adjustments, such as limiting sugary foods, can help ease these symptoms.
- Avoid greasy, fried, or spicy foods, which can worsen nausea.
- Eat small, frequent meals to avoid overwhelming the stomach.
- Stay hydrated—water and electrolyte-rich fluids help with digestion and nausea.
3. Supports Gut Health
Because semaglutide affects gastric motility (slows down how fast food moves through your stomach), foods that support digestion become even more critical.
- High-fiber foods (in moderation) like oats, chia seeds, and leafy greens promote regularity.
- Probiotic-rich foods (yogurt, kefir, sauerkraut) may help balance gut flora.
4. Prevents Nutritional Deficiencies
Semaglutide can significantly reduce appetite, which helps with weight loss. But in some cases, this can lead to eating too little. A diet that’s too low in calories may result in:
- Protein deficiency
- Electrolyte imbalances
- Micronutrient shortfalls such as B12, iron, or magnesium
Tip: Ensure meals include a variety of macro- and micronutrients to support metabolism and energy levels.
5. Improves Long-Term Success
Semaglutide is not a stand-alone solution. A balanced diet builds long-term habits that support weight maintenance after stopping the medication and can also help control insulin production .
- People who pair semaglutide with diet and lifestyle changes are more likely to keep weight off and avoid weight regain after discontinuation.
What Not To Eat When Taking Semaglutide
While semaglutide doesn’t come with a strict diet, your food choices can make a big difference in how effective and tolerable it is. This guide covers which foods to avoid or limit and why those choices matter.
1. Fried and Greasy Foods
Semaglutide slows gastric emptying (how quickly food leaves your stomach). Fried and greasy foods are already tough to digest. They can intensify common side effects like nausea, bloating, heartburn, and stomach cramps, especially in the early weeks of treatment, making it essential to consult an obesity medicine specialist. These foods also tend to be calorie-dense and nutrient-poor, making them counterproductive for weight management.
Examples:
- Fried chicken
- French fries
- Fast food burgers
- Bacon and sausage
- Heavy cream-based pasta or casseroles
Tip: Choose grilled, baked, or steamed options, and use heart-healthy oils like olive oil in moderation.
2. High-Sugar Foods and Beverages
Semaglutide helps regulate blood sugar. Consuming high-sugar foods can spike blood sugar levels, leading to energy crashes and undermining the drug’s purpose. These items also contribute to excessive calorie intake without satiety, which can stall or reverse weight loss progress.
Examples:
- Candy, cookies, cakes, doughnuts
- Regular sodas and sugary drinks
- Sweetened breakfast cereals
- Syrups, sweet coffee drinks, and milkshakes
Tip: Satisfy sweet cravings with fruit, dark chocolate (in moderation), or yogurt sweetened with berries.
3. Refined Carbohydrates
Refined carbs are quickly digested and offer minimal fiber, causing blood sugar spikes and crashes. They don’t promote satiety, which can lead to overeating despite semaglutide’s appetite-reducing effects.
Examples:
- White bread and white rice
- Regular pasta
- Many crackers and pretzels
- Pastries and refined-flour baked goods
Tip: Swap for whole-grain alternatives like brown rice, quinoa, whole wheat bread, or legumes.
4. Carbonated Beverages
Even non-caloric options like sparkling water, along with drinking alcohol, can worsen bloating, gas, and abdominal discomfort, symptoms already common with semaglutide due to slowed digestion.
Examples:
- Regular or diet soda
- Sparkling water (especially flavored or artificially sweetened)
- Beer and other fizzy alcoholic drinks
Tip: Stay hydrated with flat water, herbal teas, or water infused with citrus, mint, or cucumber.
5. Alcohol
Alcohol has multiple interactions with semaglutide:
- It can increase the risk of hypoglycemia, especially in those also using insulin or sulfonylureas.
- It may worsen nausea or digestive issues.
- It’s high in empty calories and can impair judgment, leading to overeating or poor food choices.
Examples:
- Cocktails with sugary mixers
- Sweet wines or liqueurs
- Beer (mainly due to carbonation and carbs)
Best Practices:
- Avoid alcohol on an empty stomach.
- Limit intake and choose lower-sugar options like dry wine or liquor mixed with soda water.
6. Highly Processed Foods
Processed foods often contain excess sodium, added sugars, artificial ingredients, and unhealthy fats. These contribute to poor blood sugar control, cravings, and inflammation—all of which can work against semaglutide’s benefits.
Examples:
- Packaged snacks like chips, cookies, or snack cakes
- Instant ramen and boxed meals
- Frozen pizzas or microwave dinners
- Processed meats (hot dogs, bacon, deli meats)
Tip: Focus on whole, minimally processed foods—lean proteins, fresh produce, whole grains, nuts, and seeds.
7. Large Meals
Semaglutide delays stomach emptying, which helps you feel full longer. Eating large meals can overwhelm the stomach, leading to excessive fullness, nausea, acid reflux, or vomiting, which is why it’s important to avoid foods that could exacerbate these issues.
Better Strategy:
- Eat smaller, more frequent meals (4–6 per day if needed).
- Take your time chewing and eating slowly.
- Stop eating when you feel about 80% full to avoid discomfort later.
Bonus Tips for Eating Well on Semaglutide
- Stay hydrated: Dehydration can worsen nausea. Aim for 8+ cups of water daily.
- Prioritize protein: It supports satiety and muscle maintenance. Include lean meats, tofu, eggs, or legumes at each meal.
- Eat fiber-rich foods: These help regulate digestion and blood sugar.
- Track your symptoms: Keeping a food diary can help identify triggers.
How To Eat Smarter On Semaglutide
Eating smarter on semaglutide isn’t about following a strict set of rules. It’s about making choices that help you feel better, avoid common side effects, and stay on track. A few simple habits can go a long way:
1. Focus on High-Quality Protein
Protein promotes satiety, stabilizes blood sugar, supports lean muscle mass, and helps counteract the appetite-reducing effects of semaglutide (which can sometimes lead to under-eating), making non-fat dairy products potentially a better choice than full fat options.
How to include it:
- Aim for 20–30g of protein per meal.
- Combine animal and plant sources for variety.
Examples:
- Chicken, turkey, fish, eggs
- Greek yogurt, cottage cheese
- Lentils, tofu, tempeh, edamame
- Protein shakes (low in sugar)
2. Prioritize Fiber-Rich Foods
Fiber supports digestion, helps regulate blood glucose, and keeps you full longer, working synergistically with semaglutide.
How to include it:
- Choose whole fruits and vegetables, especially those with edible peels.
- Opt for whole grains and legumes over refined carbs.
Examples:
- Berries, apples, pears, carrots, broccoli
- Oats, brown rice, quinoa, barley
- Chickpeas, black beans, lentils
Tip: Increase fiber gradually and hydrate well to reduce bloating or discomfort.
3. Eat Small, Balanced Meals
Semaglutide slows digestion, and large or heavy meals, especially those high in fatty foods, can cause nausea, early fullness, bloating, or reflux.
How to implement:
- Split meals into 4–6 smaller portions per day if needed.
- Use the “50/25/25 rule” for meal planning: 50% non-starchy veggies, 25% lean protein, 25% whole grains or starchy veg.
Sample meal:
Grilled salmon + roasted broccoli + quinoa + a squeeze of lemon.
4. Eat Slowly and Mindfully
It takes time for your brain to register fullness. Semaglutide enhances satiety signals, so eating slowly helps you tune in and prevent overeating or nausea.
Strategies:
- Put your fork down between bites.
- Chew thoroughly.
- Avoid screens during meals and eat without rushing.
- Stop eating when you feel about 80% full.
5. Stay Consistently Hydrated
Semaglutide can reduce thirst cues. Dehydration may worsen nausea, headaches, and fatigue.
Tips:
- Aim for 8–10 cups of water daily, more if active or in hot weather.
- Include herbal teas, broths, or water with lemon/cucumber/mint.
- Monitor urine color—pale yellow is ideal.
6. Limit Trigger Foods
Certain foods are not “forbidden” but can aggravate side effects or counteract semaglutide’s benefits.
Limit or avoid:
- Fried, greasy, or creamy dishes
- Sugary snacks and beverages
- White/refined carbs (white bread, pastries)
- Carbonated drinks (bloating)
- Alcohol (stomach upset, low blood sugar risk)
7. Don’t Skip Meals (Even If You’re Not Hungry)
Semaglutide suppresses appetite, but under-eating can lead to fatigue, nutrient deficiencies, or muscle loss.
Tips:
- Set meal reminders if needed.
- Choose nutrient-dense mini meals if appetite is low (e.g., a boiled egg, a few nuts, or yogurt with berries).
8. Plan Ahead and Meal Prep
Having smart, pre-portioned meals reduces impulsive choices and ensures you’re eating nutrient-rich food that supports your goals.
Ideas:
- Prepare grain bowls, salads, or stir-fries in advance.
- Freeze high-protein soups or stews.
- Keep snack boxes with nuts, boiled eggs, cut veggies, or hummus.
9. Track Your Symptoms and Triggers
Everyone’s tolerance is different. Tracking what you eat and how you feel can help fine-tune your diet.
Track:
- Meal timing and portions
- Foods that worsen or ease symptoms
- Bowel habits, nausea, fatigue
- Hunger/fullness cues
10. Talk to a Dietitian or Your Healthcare Provider
Personalized guidance can help you meet your nutrition needs without triggering symptoms. A professional can also help if you’re experiencing excessive appetite loss or weight loss plateaus.