If you have started taking semaglutide and noticed that your nights are more restless, you are not alone. Many patients report experiencing insomnia, and while not everyone reacts the same way, the disruption can feel frustrating. Semaglutide can subtly influence your body’s sleep-wake rhythm, affecting how easily you fall asleep or stay asleep through the night.
With the right sleep tips for people experiencing semaglutide insomnia, you can ease nighttime restlessness, support your body’s natural recovery, and build habits that promote restful sleep.
How Can Semaglutide Affect Sleep?
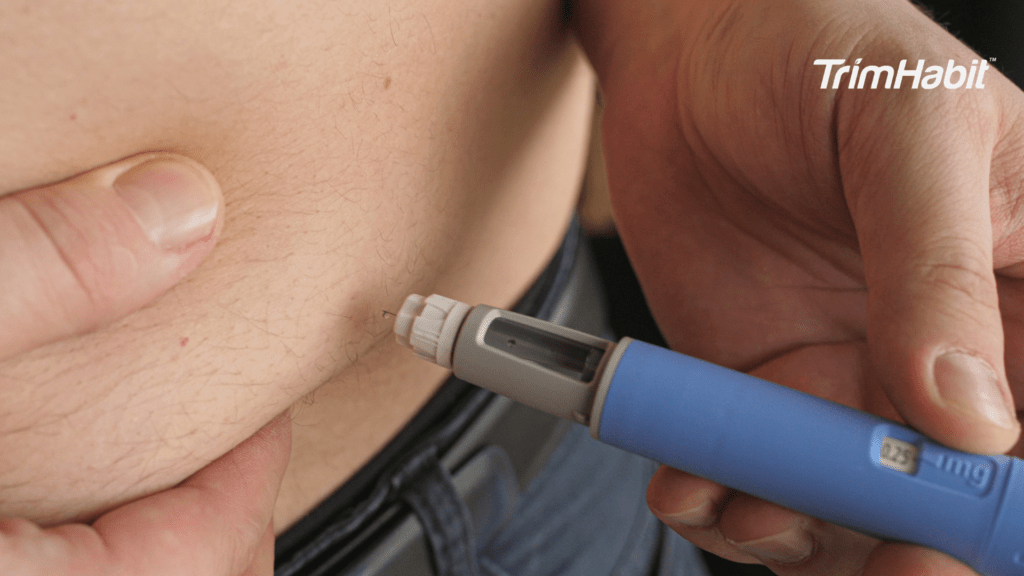
Semaglutide is a GLP-1 receptor agonist that helps with weight management, regulating appetite, and controlling blood sugar levels. Although it offers therapeutic benefits, some people also notice that taking semaglutide affects how easily they can fall asleep or stay asleep1,2. For some, this is temporary as the body adjusts, but for others the changes in sleep patterns last longer and may require closer attention.
Sleep disturbances linked with semaglutide are not fully understood. They may relate to shifts in brain activity, gastrointestinal issues, or the drug’s influence on insulin release and insulin secretion. Because individual responses vary, you may find your nights disrupted while others experience significant improvements. Existing research is still limited, and further research is needed to explain why semaglutide and insomnia appear connected for some people.
How Does Weight Loss Affect Sleep Quality?
Weight loss can bring both benefits and challenges for your sleep. As your body becomes lighter, you may notice fewer sleep disturbances and improved sleep quality, especially if you previously had sleep apnea or related breathing problems. The reduced pressure on your airway can make breathing easier at night, helping you wake up more refreshed.
However, during active weight loss, hormonal shifts that regulate appetite and metabolism can temporarily affect sleep patterns, making it harder to fall asleep or stay asleep. Your body is adapting to changes in energy use, insulin release, and blood sugar balance. For people managing diabetes, these shifts can make nighttime awakenings or restlessness more noticeable.
Focusing on a balanced diet, gentle physical activity, and a consistent bedtime routine can help your body adjust. Over time, as your metabolism stabilizes and your body finds its new rhythm, you may experience more restful sleep and steadier energy throughout the day.
Are Sleep Problems Common In People Managing Diabetes?
If you are managing diabetes, you face a higher likelihood of developing sleep disorders compared with the general population. This is partly because unstable blood sugar levels can influence sleep patterns, leading to both nighttime awakenings and daytime fatigue. When blood glucose runs too high, you may wake up frequently to use the bathroom or feel restless. On the other hand, if levels drop too low during the night, your body can respond with symptoms such as sweating, headaches, or vivid dreams, all of which can disrupt sleep.
Another concern is the connection between diabetes and conditions like sleep apnea and obstructive sleep apnea (OSA). OSA occurs when the muscles in your airway collapse during sleep, causing breathing pauses that repeatedly wake you up throughout the night. Many people with type 2 diabetes experience OSA symptoms such as loud snoring, gasping for air, and morning headaches. These interruptions not only fragment your rest but also affect sleep patterns over time, leaving you feeling unrefreshed even after a full night in bed.
Good diabetes management can lessen these risks by helping regulate blood sugar levels, which can stabilize sleep. However, even with careful management, some diabetes medications and other drugs can have adverse effects that influence sleep patterns, ranging from difficulty falling asleep to frequent nighttime awakenings. Because of this, it is not unusual for people with diabetes to report sleep disturbances, and recognizing the link can help you address the problem more effectively.
What Contributing Factors Make It Harder To Sleep?
When you are experiencing insomnia, it is rarely caused by a single issue. Instead, several contributing factors tend to interact and make sleep more elusive. One of the most common is fluctuating blood glucose. High levels can make you feel jittery or restless, while low levels may cause symptoms that wake you up, such as sweating or dizziness. Over time, these fluctuations can affect sleep and lead to chronic insomnia if left unmanaged.
Changes in appetite and gastrointestinal issues associated with taking semaglutide may also play a role. For example, nausea or fullness in the evening can make it harder to relax, while late-night snacking triggered by hunger swings may disrupt the body’s normal circadian rhythm. Stress is another powerful factor. When you are worried about your health, diet, or diabetes management, your brain activity remains heightened at night, making it harder to fall asleep or stay asleep.
The body’s internal clock strongly influences when you feel tired or alert. If your sleep schedule is irregular or if you are exposed to bright light from screens late in the evening, this circadian rhythm can shift and affect sleep patterns in ways that make it harder to wind down. Lifestyle changes such as poor diet choices, reduced physical activity, or skipping stress management practices may worsen sleep disturbances.
Even your medical history and the other medications you take can affect how easily you achieve restful sleep. Conditions like cardiovascular disease, depression, or gastrointestinal problems are all linked to sleep issues, while some other diabetes medications and unrelated drugs may cause side effects like restlessness or vivid dreams. Because multiple contributing factors often overlap, it is helpful to look at the full picture when trying to understand your sleep challenges.
Practical Sleep Tips For People Experiencing Semaglutide Insomnia
The good news is that you have practical steps available for managing insomnia. Below are science-informed sleep tips for people experiencing semaglutide insomnia:
- Follow a consistent sleep schedule. Going to bed and waking up at the same time each day trains your body’s internal clock and helps you avoid chronic insomnia. Over time, this consistency encourages better sleep quality.
- Build a relaxing bedtime routine. Activities such as reading, warm showers, or deep breathing exercises can calm your mind and body. Gentle yoga and other soothing activities signal your brain receptors that it is time to rest, which makes it easier to fall asleep.
- Create good sleep hygiene habits. Keep your bedroom cool, dark, and quiet, and avoid screens before bed. Limiting caffeine and alcohol close to bedtime is another cornerstone of good sleep hygiene that can improve sleep.
- Manage blood sugar levels. Unstable blood glucose can cause sleep disturbances, so pairing a healthy diet with proper diabetes management is crucial. Staying mindful of your evening meals, including whole foods and smaller portions, helps regulate blood sugar levels overnight and promote restful sleep.
- Use lifestyle changes to enhance sleep. Exercise during the day, stress reduction techniques, and managing weight loss all contribute to improved sleep quality. While vigorous workouts late at night can affect sleep, daytime movement supports your circadian rhythm and can promote better sleep.
- Address other health conditions. Sleep disturbances may be linked to cardiovascular disease, obesity, or OSA symptoms. If you experience sleep apnea, talk to your healthcare provider about treatment options. Tackling these issues not only supports better sleep quality but also helps with overall health and weight loss.
- Seek professional guidance. If sleep issues continue, consult healthcare professionals. Sleep specialists can evaluate whether you are experiencing sleep disturbances from semaglutide itself or if other medications, medical history, or underlying conditions are the main cause. They may adjust your treatment, consider other diabetes medications, or suggest strategies tailored to your needs.
Why Does This Matter For Your Health?
Not getting enough sleep can affect sleep quality the next day and lead to fatigue, trouble focusing, and reduced energy. Over time, chronic insomnia and unmanaged sleep problems may increase the risk of cardiovascular disease. Because semaglutide involves complex interactions with brain activity, gastrointestinal issues, and appetite regulation, it can affect sleep in unique ways that other diabetes medications or other drugs may not.
Improved sleep quality is possible when you address both the medical and lifestyle sides of the problem. Managing insomnia, practicing sleep hygiene, and talking with healthcare professionals ensures you can experience the benefits of semaglutide without compromising your rest.
Final Thoughts
While semaglutide and insomnia may be connected for some, remember that individual responses vary. For many people, sleep disturbances ease as the body adjusts. For others, contributing factors like blood sugar fluctuations, OSA symptoms, or stress make it harder to achieve restful sleep. With the right lifestyle changes, better sleep habits, and support from your healthcare provider, you can reduce sleep issues, enhance sleep, and maintain both better sleep quality and effective diabetes management.