Semaglutide, a medication commonly prescribed for managing type 2 diabetes and aiding in weight loss, has become increasingly popular for its effectiveness. However, like many medications, it can come with side effects—one of the most frequent being constipation.
This uncomfortable symptom can interfere with daily life and discourage people from staying on treatment. Fortunately, a healthy diet plays a decisive role in managing digestive issues.
This article discusses foods that help with constipation while taking semaglutide, offering practical tips to support your gut health and treatment journey.
What Is Semaglutide?
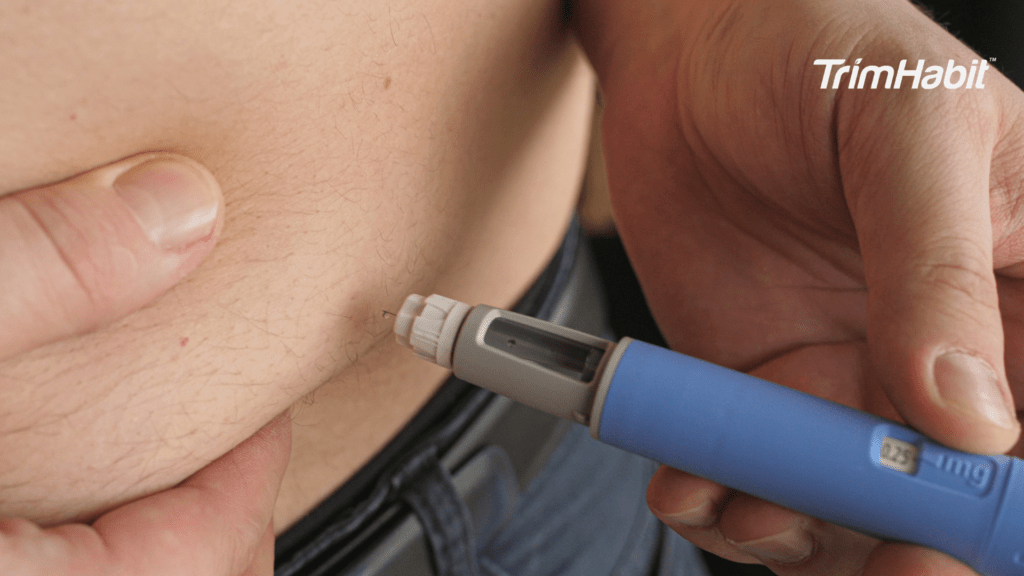
Semaglutide is a GLP-1 receptor agonist, a class of medications that mimics the action of glucagon-like peptide-1 (GLP-1), a hormone that helps regulate blood sugar and appetite. Depending on its use and formulation, it is available under brand names such as Ozempic, Wegovy, and Rybelsus1.
Approved Uses
- Type 2 Diabetes (Ozempic, Rybelsus)
- Helps control blood glucose levels2.
- Often used alongside diet, exercise, or other diabetes medications2.
- Chronic Weight Management (Wegovy)
- Approved for adults with obesity or overweight with at least one weight-related condition (e.g., hypertension, type 2 diabetes, or high cholesterol).
- Supports significant and sustained weight loss when combined with lifestyle interventions.
How It Works
- Increases insulin secretion (only when blood sugar is high).
- Suppresses glucagon secretion (a hormone that raises blood sugar).
- Slows gastric emptying, making people feel full longer.
- Reduces appetite and food intake through actions in the brain.
Effectiveness
- Diabetes: Helps reduce HbA1c and supports weight loss3.
- Weight Loss: Clinical trials show average body weight reductions of 10–15% or more, depending on the dose and duration4.
Side Effects
Common:
- Nausea
- Vomiting
- Diarrhea
- Constipation
- Stomach cramps
Serious (rare):
- Pancreatitis
- Gallbladder issues
- Risk of thyroid C-cell tumors (in animal studies)
Considerations & Contraindications
- Not for type 1 diabetes or diabetic ketoacidosis.
- Avoid in people with a history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2.
- Caution with gastrointestinal disorders or when taking other weight-loss medications.
Lifestyle Integration
- Works best with a balanced diet, regular physical activity, engaging in light exercises like daily walks, and behavioral changes. Consulting with healthcare providers for personalized guidance can enhance digestive health and promote healthy bowel movements5.
- Should be part of a long-term, comprehensive approach to health management6.
Foods That Help With Constipation While Taking Semaglutide
When taking semaglutide (Ozempic, Wegovy, or Rybelsus), constipation is a common side effect due to slowed gastric emptying. Choosing the right foods can help alleviate constipation and relieve this issue without worsening nausea or bloating, which are also common with semaglutide.
Here’s a list of gentle, effective foods to support digestion and relieve constipation while taking semaglutide:
1. Cooked Vegetables (Well-Softened)
Cooked veggies are easier to digest than raw and still provide fiber. Good options include steamed zucchini, carrots, spinach, green beans, roasted sweet potatoes, or squash.
2. Oats and Oat Bran
These are rich in soluble fiber (beta-glucan), which helps soften stool. Warm oatmeal with chia or flax seeds can be a gentle and effective option.
3. Chia Seeds and Ground Flaxseeds
Both are rich in soluble fiber and omega-3s, helping to form gel-like stool and support bowel movements. Add them to oatmeal, yogurt, or smoothies.
4. Prunes and Prune Juice
Prunes contain fiber, sorbitol, and natural compounds that stimulate digestion. A few prunes or half a cup of juice daily can help ease constipation and soften stools.
5. Kiwi
Kiwi is high in fiber and contains actinidin, an enzyme that supports digestion. It can help improve stool consistency and make bowel movements more regular.
6. Pears and Apples (with Skin)
These fruits provide pectin (a soluble fiber) and a mild dose of sorbitol. Baked versions are good if raw fruits cause discomfort.
7. Hydrating Fruits
Staying hydrated through food helps maintain stool softness. Good choices include cucumber, watermelon, oranges, grapes, and berries. Additionally, drinking plenty of water is essential for preventing and alleviating the side effects of semaglutide. Proper hydration supports digestive health, particularly in preventing constipation. Aim to drink a certain daily intake of water to maintain optimal functioning.
8. Whole Grains (In Moderation)
Whole grains like brown rice, quinoa, whole wheat toast, and barley provide insoluble fiber that adds bulk to the stool. Introduce gradually to avoid gas.
9. Low-Fat Yogurt with Probiotics
Probiotic-rich yogurt supports gut bacteria and may improve stool frequency. Look for brands with live cultures like Lactobacillus or Bifidobacterium.
10. Water and Herbal Teas
Adequate hydration is essential for fiber to function well. Herbal teas like peppermint, ginger, or dandelion root can support digestion and relaxation.
Additional Tips For Managing Constipation Naturally
Here are additional natural tips for managing constipation effectively, beyond nutrients and food components:
Establish a Consistent Bathroom Routine
- Go when you feel the urge – delaying can lead to harder stools.
- Try to have a regular time each day, such as after breakfast.
Increase Physical Activity
- Movement stimulates gut motility, helping stool move through the colon and enhancing digestive health.
- Aim for at least 30 minutes of moderate activity daily (e.g., walking, yoga, swimming) to support digestive health.
- Abdominal massage or gentle yoga poses (like wind-relieving pose) can also help.
Improve Toilet Posture
- Use a footstool or squatting position to straighten the rectal canal.
- This aligns the body for easier elimination and reduces strain.
Practice Stress Management
- Chronic stress can negatively affect digestion and slow bowel function.
- Consider mindfulness, deep breathing, meditation, or progressive muscle relaxation.
Try Warm Liquids in the Morning
- A cup of warm water, herbal tea, or lemon water may stimulate the bowels.
- Some people benefit from coffee due to its natural stimulatory effect.
Chew Food Thoroughly and Eat Mindfully
- Proper chewing begins digestion and eases the work of the intestines.
- Avoid rushed meals; eat slowly and avoid distractions while eating.
Avoid Overuse of Laxatives
- While over-the-counter laxatives may provide relief, chronic use can lead to dependency. Mild laxatives can be an option for individuals experiencing constipation when natural remedies and lifestyle changes are insufficient. However, it is important to consult a healthcare provider before using these products to ensure safety and appropriateness, and to avoid disruptions to normal bowel function.
- Focus on dietary fiber, hydration, and lifestyle as long-term solutions.
Keep a Bowel Movement Journal
- Track frequency, consistency (using the Bristol Stool Chart), diet, fluid intake, and any symptoms.
- Helps identify triggers or patterns and supports better discussion with healthcare providers.
Stay Cool on Low-Fiber Diets
- If you’re following a low-fiber diet (e.g., for IBS, SIBO, or after surgery), focus on:
- Hydration
- Gentle movement
- Osmotic support like magnesium or prune juice (if allowed)
Try Natural Remedies (with Caution)
- Aloe vera juice, slippery elm, or tripahala (Ayurvedic herb) are sometimes used but should be taken with professional guidance.
- Always consult with a healthcare provider before starting herbal remedies, especially if pregnant, elderly, or on medication.
When To Seek Medical Help
Constipation is common, especially when starting medications like semaglutide, but it shouldn’t be ignored if it becomes severe or persistent. Medical evaluation may be necessary if:
Constipation Lasts More Than a Week
- If you’re not having regular bowel movements for more than 7 days, despite dietary and lifestyle efforts.
You Have Severe Abdominal Pain or Bloating
- Especially if pain is sudden, sharp, or persistent, or if you’re unable to pass gas.
Nausea or Vomiting Occurs
- These may indicate a bowel obstruction, which requires immediate attention.
You Notice Blood in the Stool
- Bright red blood may suggest hemorrhoids, but dark or tarry stools could signal bleeding higher in the digestive tract.
You Experience Unintentional Weight Loss
- Especially if accompanied by a change in bowel habits or appetite loss.
You Have a History of GI Disorders
- If you have IBS, IBD, diverticulitis, or colon polyps, and constipation suddenly worsens.
Over-the-Counter Remedies Don’t Help
- If stool softeners, fiber supplements, or dietary changes have no effect after several days.
You Develop a New or Worsening Symptom While on Semaglutide
- This includes severe dehydration, worsening nausea, cramping, or signs of pancreatitis (e.g., pain radiating to the back, fever, or vomiting).
You Can’t Pass Stool or Gas at All
- This could indicate a serious blockage or impaction and needs urgent care.
You’re Over 50 and Experiencing New Bowel Changes
- Any new or unexplained change in bowel patterns in older adults should be checked to rule out colon cancer or other conditions.