Starting semaglutide can be an exciting step toward better health, since it helps with weight loss and managing type 2 diabetes. As your body adjusts, you may notice side effects such as acid reflux. That burning sensation in your chest or throat can be discouraging, especially when you are trying to stay consistent with your medication and nutrition plan. The good news is that you are not alone, and there are practical ways to ease the discomfort and keep moving forward.
In this article we’ll explore dealing with acid reflux while on semaglutide, effective strategies to help you feel more comfortable while staying on track with your goals.
Understanding Semaglutide, Stomach Acid, And Acid Reflux
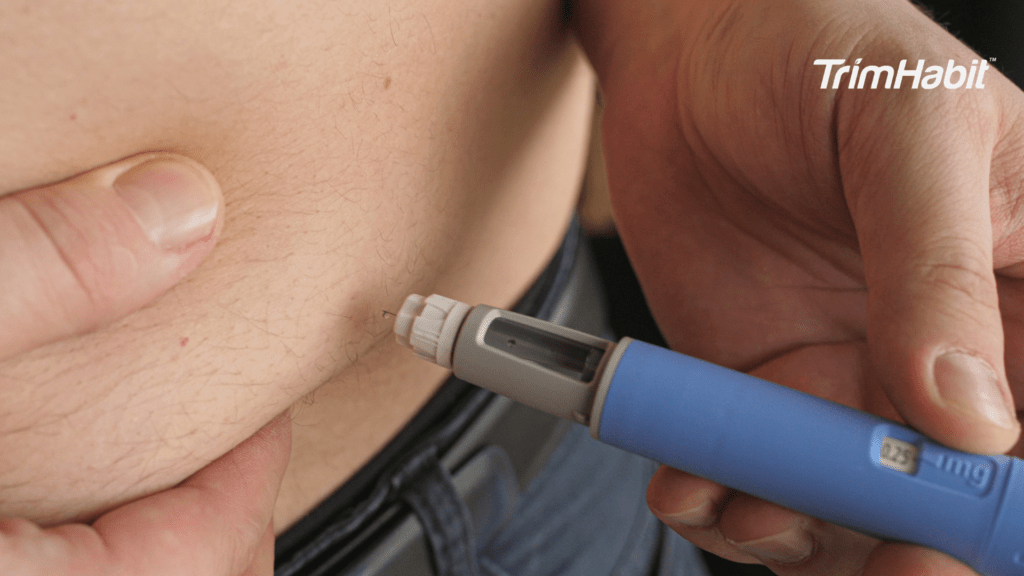
Semaglutide has become a widely used medication for type 2 diabetes and weight management, thanks to its ability to regulate blood sugar levels and curb appetite. As a key tool in diabetes management, semaglutide helps lose weight by reducing appetite and lowering overall caloric intake. Semaglutide is often administered as semaglutide injections1. Semaglutide injections can sometimes cause or worsen acid reflux symptoms because they may delay stomach emptying, which increases the risk of reflux.
However, you may notice new or worsening digestive issues after starting semaglutide, and acid reflux is one of the most common. Acid reflux is a common side effect observed in clinical trials of semaglutide. That burning discomfort in the chest or throat can feel discouraging, especially when trying to stay consistent with your treatment. Understanding why this happens and how to manage it can help you stay on track with your health goals2.
Why Semaglutide Can Trigger Acid Reflux
- Delayed stomach emptying (gastroparesis): Semaglutide slows down how quickly food leaves the stomach, so food stays in the stomach longer, increasing the risk of reflux. This delayed emptying can cause stomach contents and excess acid to remain in the stomach, making it more likely for acid to flow back into the esophagus3.
- Changes in appetite and eating habits: Eating smaller meals or less frequently may change stomach acid levels4. Changes in meal frequency or size can also influence how much acid the stomach produces, which may contribute to acid reflux symptoms.
- Increased digestive tract sensitivity: Some people naturally experience more irritation as their GI system adjusts. This can result in discomfort or a burning feeling in the chest or throat. Chronic acid reflux is known as gastroesophageal reflux disease (GERD), which can have long-term health implications2.
Understanding The Digestive System And Reflux
The digestive system is a complex network designed to break down food and absorb nutrients, but it can also be sensitive to changes especially when medications like semaglutide are involved. When you eat, food travels down the esophagus and passes through the lower esophageal sphincter (LES), a muscular ring that acts as a gatekeeper between the esophagus and the stomach. Usually, the LES closes tightly after food enters the stomach, preventing stomach acid from flowing back up.
Recognizing Acid Reflux Symptoms
Acid reflux happens when stomach acid flows back into the esophagus, irritating it. While occasional reflux is common, frequent or persistent symptoms can affect quality of life and may need medical attention. Knowing the signs makes it easier to manage the condition early.
Common Symptoms
- Heartburn symptoms – A burning feeling or sensation in the chest or throat, often after meals or at night.
- Regurgitation – A sour or bitter taste in the mouth when stomach acid backs up.
- Bloating or fullness – Feeling uncomfortably full even after small meals.
- Difficulty swallowing (dysphagia) – The sensation of food sticking in the throat or chest.
- Nausea – Sometimes mild, but may overlap with heartburn.
- Chronic cough or throat irritation – Caused by acid irritating the throat or vocal cords.
Less Obvious Symptoms
- Hoarseness or voice changes
- Bad breath (halitosis)
- Chest pain that mimics heart issues (essential to rule out cardiac causes)
- Frequent hiccups
- Excessive burping
When to Seek Help: If reflux symptoms occur more than twice a week, disturb your sleep, or come with alarming signs such as vomiting blood, black stools, or unintentional weight loss, consult a healthcare provider.
Dietary Triggers For Reflux
What you eat and how you eat can have a significant impact on acid reflux, especially when taking semaglutide. Certain foods trigger reflux symptoms by increasing acid production, irritating the stomach lining, or slowing gastric emptying.
Spicy foods, for example, can irritate the digestive tract and trigger reflux. In contrast, fatty foods tend to linger in the stomach, increasing the risk that stomach acid will back up into the esophagus.
Citrus and other acidic fruits, such as oranges, lemons, and tomatoes, can also increase acid production and worsen reflux symptoms. For many, these foods are common triggers that make managing acid reflux more challenging. Eating large meals or going long stretches without eating can also put extra pressure on your stomach, making it easier for acid to escape.
Dealing With Acid Reflux While On Semaglutide
Managing acid reflux often goes beyond medication, and small daily changes can make a big difference. These adjustments can help reduce the backflow of stomach acid and keep your symptoms under control:
1. Eat Smaller, More Frequent Meals – Large meals put extra pressure on the stomach, increasing the chance of acid pushing upward. Smaller, balanced portions are easier to digest.
2. Avoid Trigger Foods and Drinks – Spicy, fried, fatty, and acidic foods (like tomatoes or citrus) can worsen reflux. Coffee, alcohol, and carbonated drinks may also aggravate symptoms.
3. Maintain a Healthy Weight – Excess weight around the midsection adds pressure to the stomach, which can push acid into the esophagus. Even modest weight loss may improve symptoms.
4. Stay Upright After Eating – Lying right after a meal makes reflux more likely. Wait 2–3 hours before lying down or going to bed.
5. Elevate Your Head While Sleeping – Raising the head of your bed by 6–8 inches (or using a wedge pillow) helps gravity keep stomach acid down at night by elevating the upper body, preventing acid from flowing back into the esophagus.
6. Avoid Tight Clothing – Tight clothing, especially around the waist, can increase pressure on the stomach and worsen reflux. Choose loose-fitting garments to help reduce discomfort.
7. Practice Mindful Eating – Eating slowly, chewing thoroughly, and avoiding overeating can ease digestion and reduce discomfort.
8. Quit Smoking (if applicable) – Smoking relaxes the lower esophageal sphincter (LES), making it easier for acid to flow upward.
9. Manage Stress – Stress doesn’t directly cause reflux, but can worsen symptoms. Deep breathing, walking, or mindfulness techniques may help.
10. Carry Water, Sip Often – Keeping a water bottle nearby helps you stay hydrated without overfilling your stomach at once. Small sips are better than big gulps.
11. Schedule Movement After Meals – A short walk after eating can encourage digestion and reduce pressure that leads to reflux.
12. Pack Snacks Wisely – Keep reflux-friendly snacks on hand like apple slices, rice cakes, or nuts to avoid being tempted by trigger foods when hunger hits.
13. Try Ginger Tea – Ginger tea is a soothing beverage that may help calm your stomach and ease reflux symptoms, thanks to its natural anti-inflammatory properties.
14. Set an Evening Cut-Off – Try to finish dinner 2–3 hours before bed. Choose something light for a nighttime bite, like a banana or whole-grain toast.
15. Keep a Symptom Journal – Tracking what you eat, when you take semaglutide, and when reflux symptoms flare up can help you notice patterns and give your doctor valuable details to guide your care.
Medical Strategies And Support
While lifestyle changes can go a long way in reducing reflux, you may still need additional medical strategies, including stronger medications, to keep symptoms under control. This is especially true if you are taking semaglutide, since it affects digestion.
1. Over-the-Counter (OTC) Options
- Antacids – Provide quick relief by neutralizing stomach acid (e.g., calcium carbonate).
- H2 Blockers – Reduce acid production and can last longer than antacids (e.g., famotidine).
- Proton Pump Inhibitors (PPIs) – Stronger acid reducers often used for persistent reflux (e.g., omeprazole). These medications work to reduce stomach acid and help control reflux symptoms.
2. Prescription Treatments. If OTC options aren’t enough, a doctor may prescribe more potent medications or higher doses, such as higher-strength H2 blockers, PPIs, or more potent medications tailored to your needs. Sometimes, higher doses are necessary to manage symptoms better, but your provider will monitor for any changes or side effects.
3. Adjusting Semaglutide Use. Sometimes, your healthcare provider may:
- Lower the dose temporarily
- Change the timing of your injection
- Suggest supportive medications to ease digestion
4. Monitoring for Complications. Persistent reflux can lead to untreated esophagitis, ulcers, or Barrett’s esophagus. Regular check-ins with a healthcare provider help catch issues early.
5. Professional Support
- Gastroenterologist care – For ongoing or severe reflux.
- Dietitian guidance – To create a reflux-friendly diet that aligns with Semaglutide goals.
- Pharmacist input – To ensure safe use of acid-reducing medications alongside other prescriptions.
When To Call Your Doctor
While occasional acid reflux can be managed with lifestyle changes and over-the-counter remedies, there are times when medical attention is important. Knowing when to reach out ensures that small issues don’t become bigger health problems.
Call your doctor if you experience:
- Reflux symptoms more than twice a week, despite adjustments
- Persistent or worsening heartburn that interferes with daily life
- Difficulty swallowing or the feeling that food is stuck in your throat
- Unexplained weight loss, fatigue, or loss of appetite
- Chronic cough, hoarseness, or sore throat not linked to a cold or allergies
- Chest pain that could be confused with heart issues (always rule out cardiac causes urgently)
Seek immediate medical care if you notice:
- Vomiting blood or material that looks like coffee grounds
- Black, tarry stools
- Severe chest or abdominal pain
Conclusion
Semaglutide can be a powerful tool for improving blood sugar control and supporting weight loss, but side effects like acid reflux can sometimes make the journey feel challenging. The good news is that reflux doesn’t have to derail your progress. You can stay comfortable by recognizing symptoms early, making simple lifestyle adjustments, and leaning on medical support when needed while continuing to benefit from your treatment.
If reflux becomes persistent or severe, don’t ignore it — your healthcare provider can help tailor solutions to your needs, whether adjusting your dosage, recommending supportive therapies, or addressing other underlying factors. With the right strategies, you can manage reflux effectively and stay focused on your long-term health goals.