Semaglutide, a GLP-1 receptor agonist developed initially for type 2 diabetes, has gained popularity for its appetite-suppressing and weight-reducing effects. When paired with intermittent fasting—a dietary pattern that cycles between periods of eating and fasting—the potential for enhanced results becomes even more compelling. But how do you create a sustainable and nutrient-dense diet plan that supports both?
This article discusses semaglutide and intermittent fasting meal plan, what to eat during your eating window for a balanced diet, and how to build a practical meal plan that works with your lifestyle and health goals.
What Is Semaglutide?
Semaglutide is a weight loss medication that belongs to a class of drugs called GLP-1 receptor agonists (glucagon-like peptide-1 receptor agonists)1. It is used primarily for:
- Type 2 Diabetes Management – Semaglutide helps manage type 2 diabetes by regulating blood sugar levels through various mechanisms:
- Stimulating insulin release from the pancreas when glucose levels are elevated2.
- Reducing the amount of glucose released by the liver2.
- Slowing down the rate at which food leaves the stomach (gastric emptying), which helps reduce post-meal blood sugar spikes3.
- Weight Management – In higher doses, semaglutide is also approved for significant body weight management under brand names like Wegovy4. It works by:
- Reducing appetite and calorie intake.
- Promoting feelings of fullness or satiety.
- Cardiovascular Benefits – Clinical trials have shown that semaglutide may reduce blood pressure and the risk of major cardiovascular events (like heart attack and stroke) in people with type 2 diabetes and established cardiovascular disease5.
Possible Side Effects
- Nausea, vomiting, diarrhea, constipation
- Decreased appetite
- Risk of pancreatitis (in rare cases)
- Potential thyroid tumors (seen in animal studies; relevance in humans is still being studied)
Not For:
- People with type 1 diabetes
- As a first-line treatment before other options are tried
- Those with a personal or family history of certain thyroid cancers
Basics Of Intermittent Fasting
Intermittent fasting (IF) is an eating pattern that alternates between periods of eating and fasting, which can also affect your energy levels. It focuses more on when you eat rather than what you eat6.
How It Works
During fasting periods, the body shifts from using glucose (sugar) for energy to fat burning, which is an effective method for reducing calorie intake. This metabolic switch is what gives intermittent fasting its health and weight-loss benefits7.
Common Intermittent Fasting Methods
- 16/8 Method
- Fast for 16 hours, eat within an 8-hour window
- Example: Eat from 12:00 pm to 8:00 pm
- 5:2 Diet
- Eat normally for 5 days a week
- Consume about 500-600 calories on 2 non-consecutive days
- Eat-Stop-Eat
- 24-hour fast once or twice a week
- Alternate-Day Fasting (ADF)
- Fast every other day (either complete fast or very low calorie)
- OMAD (One Meal a Day)
- Eat just one large meal per day, fast the rest
What Happens During Fasting
- 0-4 hours: Normal digestion and nutrient absorption
- 4-12 hours: Blood sugar and insulin levels start to drop
- 12-24 hours: The body begins to burn stored fat for energy (lipolysis), contributing to a calorie deficit essential for effective weight loss.
Can You Combine Semaglutide And Intermittent Fasting?
Yes, semaglutide and intermittent fasting can be combined, but this should be done with medical supervision, especially if you have underlying health conditions like type 2 diabetes or obesity8.
Here’s a breakdown of how they can work together and what to consider:
How Semaglutide and Intermittent Fasting May Complement Each Other
- Appetite Suppression
- Semaglutide reduces appetite and food intake by mimicking the GLP-1 hormone9.
- Intermittent fasting naturally reduces eating windows, which may reinforce lower calorie intake10.
- The two together can make it easier to stick to a fasting routine without feeling overly hungry.
- Improved Blood Sugar Control
- Semaglutide lowers blood glucose and improves insulin sensitivity11.
- Intermittent fasting also enhances insulin sensitivity and may reduce fasting blood glucose12.
- When combined, these effects may help stabilize blood sugar more effectively and prevent blood sugar spikes after meals13.
- Enhanced Weight Loss
- Both intermittent fasting and semaglutide independently promote fat loss14.
- In combination, they may lead to more consistent and possibly accelerated weight loss, especially in individuals with metabolic syndrome or obesity15.
Cautions and Considerations
- Risk of Low Blood Sugar (Hypoglycemia): If you are on other glucose-lowering medications in addition to semaglutide, fasting might increase your risk for hypoglycemia. Monitoring is essential4.
- Gastrointestinal Side Effects: Semaglutide commonly causes nausea, especially when starting treatment. Fasting or skipping meals might intensify this effect in some people16.
- Nutrient Intake: Intermittent fasting combined with appetite suppression might reduce overall food intake significantly. Make sure to eat nutrient-dense meals during your eating windows17. It is crucial to ensure you are receiving all essential nutrients to support overall health and metabolic function.
- Hydration: Fasting and GLP-1 medications can both suppress thirst. Be intentional about staying hydrated18.
Semaglutide And Intermittent Fasting Meal Plan
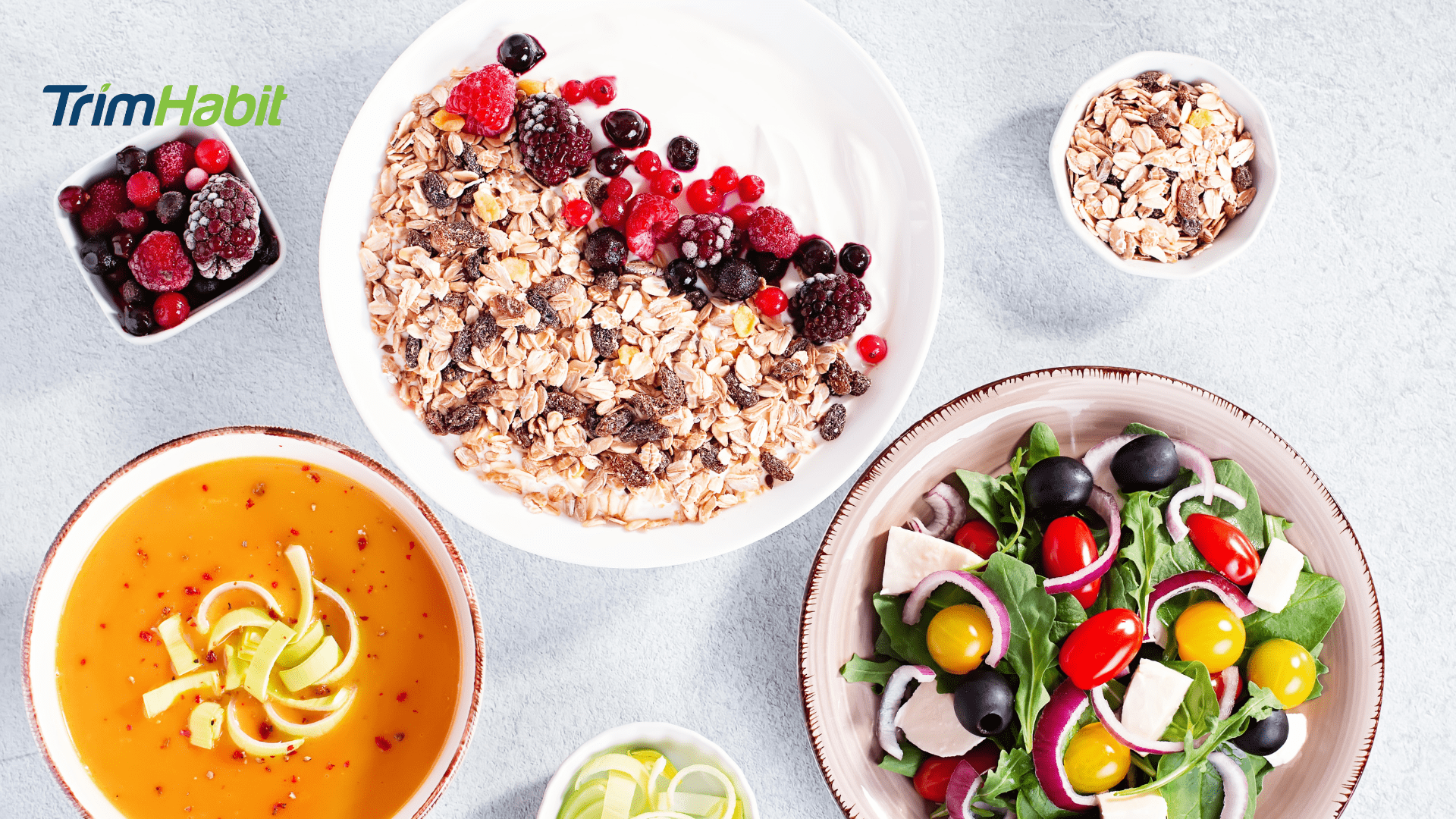
Here’s a sample meal plan that brings together a balanced diet, semaglutide, and intermittent fasting (16:8). It’s built to support steady weight loss, better blood sugar control, and nutrient-rich meals—while keeping in mind that semaglutide naturally reduces your appetite.
Assumptions:
- Eating window: 12:00 pm to 8:00 pm
- Fasting window: 8:00 pm to 12:00 pm (water, black coffee, tea allowed)
- Semaglutide injection: Typically taken once weekly; if oral, follow provider instructions (usually in the morning on an empty stomach)
- Caloric intake: Moderate (~1,200–1,600 calories/day depending on goals and body size)
- Focused on high-protein, high-fiber, low-glycemic meals to support satiety and metabolic health
Daily Sample Meal Plan
12:00 PM – Break-Fast (First Meal)
High-protein brunch bowl:
- 2 scrambled eggs + 3 egg whites
- ½ avocado
- 1 cup sautéed spinach or kale
- ¼ cup cooked quinoa or sweet potato cubes
- Drizzle of olive oil or tahini
Optional beverage: Unsweetened green tea or herbal tea
3:30 PM – Light Meal or Snack (Optional Based on Hunger)
Protein & fiber combo: Include nutrient dense whole foods in this meal for optimal health.
- ¾ cup Greek yogurt (plain, 2%)
- 1 tablespoon chia seeds or flaxseeds
- Small handful of berries or sliced cucumber + hummus
- 10-12 raw almonds or walnuts
7:30 PM – Dinner
Balanced, low-carb plate:
- 3-5 oz grilled salmon or chicken breast
- 1 cup roasted Brussels sprouts, broccoli, or cauliflower
- Side salad with olive oil & lemon dressing
- ½ cup lentils or chickpeas (optional)
Hydration Throughout the Day
- Drink plenty of water (aim for at least 6-8 cups)
- Herbal tea, sparkling water, or electrolyte water if needed
- Avoid sugary beverages and excess caffeine
Tips For Safely Combining Semaglutide And Intermittent Fasting
Pairing semaglutide with intermittent fasting can support weight loss and better blood sugar control, but it takes some planning. These practical tips can help you stay consistent, avoid common pitfalls, and make the most of both strategies.
1. Start Slowly With One Change at a Time
- Begin with either semaglutide or intermittent fasting first to let your body adjust. If you are taking semaglutide, start with small dietary changes to see how your body responds.
- Once you’re stable on one, gradually introduce the other (e.g., try a 12:12 fasting window before progressing to 16:8).
2. Stay Hydrated
- Both intermittent fasting and semaglutide can reduce thirst, increasing your risk of dehydration.
- Aim for at least 6–8 cups of water daily; add herbal teas or electrolyte-rich beverages if needed to support overall health.
3. Monitor for Hypoglycemia (Low Blood Sugar)
- If you have type 2 diabetes or take other glucose-lowering medications, fasting can increase the risk of low blood sugar.
- Watch for symptoms like dizziness, shakiness, fatigue, and irritability.
- Talk to your doctor about adjusting medications as needed.
- It’s also important to monitor high blood pressure, especially if you are dealing with obesity or other metabolic health issues. Addressing high blood pressure can significantly improve overall health and prevent diseases.
4. Prioritize Nutrient-Dense Foods
With reduced appetite from semaglutide and shorter eating windows, every bite counts. Focus on:
- Lean proteins (chicken, fish, tofu, eggs) to help maintain muscle mass
- Healthy fats (avocado, nuts, olive oil)
- High-fiber vegetables
- Whole grains and legumes in moderation
5. Avoid Overeating in the Eating Window
- Intermittent fasting doesn’t mean bingeing when the fast ends.
- Semaglutide helps reduce hunger, so follow your body’s cues and stop when satisfied. Avoid cravings for unhealthy foods by making healthier food choices during your eating window.
6. Manage Nausea Proactively
Nausea is common with semaglutide, especially early on. To minimize it:
- Break your fast with bland, small-portioned meals (e.g., eggs, yogurt, oatmeal).
- Avoid greasy, spicy, or high-fat foods.
- Avoid processed foods to minimize nausea and enhance the effectiveness of the weight-loss regimen.
- Eat slowly and chew thoroughly.
Adjust fasting duration, meal content, or semaglutide dose (with medical advice) as needed to maximize the potential health benefits.
Citations
9 Karlijn L. Kooij, Derek IJsbrand Koster, Emma Eeltink, Mieneke Luijendijk, Lisa Drost, Fabien Ducrocq, Roger A.H. Adan, GLP-1 receptor agonist semaglutide reduces appetite while increasing dopamine reward signaling, Neuroscience Applied, Volume 3, 2024, 103925, ISSN 2772-4085, https://doi.org/10.1016/j.nsa.2023.103925 (https://www.sciencedirect.com/science/article/pii/S2772408523029071)10 Duregon E, Pomatto-Watson LCDD, Bernier M, Price NL, de Cabo R. Intermittent fasting: from calories to time restriction. Geroscience. 2021 Jun;43(3):1083-1092. doi: 10.1007/s11357-021-00335-z. Epub 2021 Mar 9. PMID: 33686571; PMCID: PMC8190218.