When you first start taking semaglutide, it can feel like your appetite and your stomach suddenly start speaking different languages. One moment you feel fine, the next you’re queasy at the sight of your favorite meal.
Nausea often shows up during the early phase of treatment or after dose increases, and it can make eating feel confusing. The positive part is that this discomfort rarely lasts.
When you understand how to reintroduce foods after nausea on semaglutide, you create a smoother path forward and give your body the right kind of support.
The key is patience and curiosity. Think of it as teaching your body to trust food again. You’ll want to start with gentle flavors, simple textures, and smaller portions, letting your stomach rebuild tolerance at its own pace. You’re not just eating again, you’re retraining your digestive system to accept fuel smoothly while keeping your focus on weight management.
Why Nausea Happens On Semaglutide
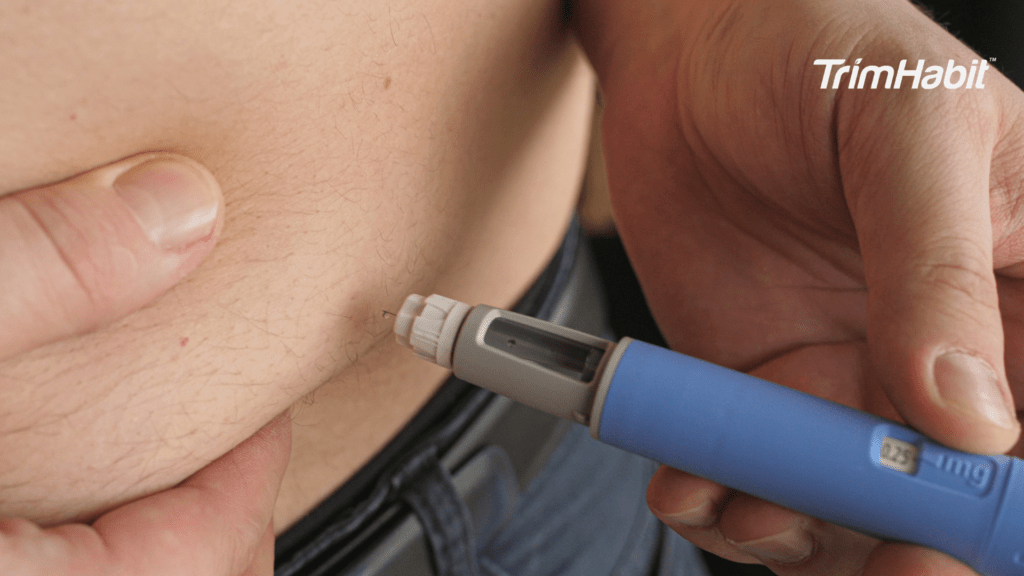
Semaglutide works as a GLP-1 receptor agonist, which means it mimics the natural hormone that helps regulate appetite and gastric emptying1. This slows how fast your stomach sends food to your intestines, giving you that longer-lasting full feeling. While this helps with weight loss, it can also make some meals sit longer than expected, sometimes causing nausea and vomiting or digestive discomfort.
In short, food doesn’t move as quickly, and that delayed movement can trigger queasiness, stomach discomfort, or bloating. As your body adjusts, these gastrointestinal symptoms usually lessen. You might even notice you can eat more types of food again after a few weeks once your body adjusts to the medication.
How To Reintroduce Foods After Nausea On Semaglutide
Step 1: Let Your Stomach Rest
If nausea hits hard, sometimes the best first move is not to push food right away. Give your stomach lining a short break and focus on hydration. Sip water or electrolyte drinks slowly. You can even try unsweetened herbal tea or clear broth if plain water feels heavy.
Avoid forcing yourself to eat when you’re queasy, especially on an empty stomach, since that can exacerbate nausea. Small sips and rest will usually help alleviate your GI symptoms.
If your nausea continues even after gentle hydration and rest, talk to your doctor about prescription anti-nausea medications that can reduce stomach discomfort without interrupting your treatment. These are sometimes recommended for people using semaglutide who experience stronger stomach reactions.
Step 2: Start with Gentle Foods
Once you feel ready to eat again, begin with bland foods that won’t irritate your stomach. Think about what’s easy on digestion and what feels safe, like crackers, rice, oatmeal, mashed potatoes, or plain toast. These are easily digestible foods that won’t overload your system.
Try eating slowly and chew thoroughly so your stomach doesn’t have to work as hard. Pair these gentle foods with hydration, and resist the urge to test your limits. Right now, you’re rebuilding trust between your body and your plate.
At this stage, avoid high-fat foods or fried foods, as they can worsen nausea or make you feel heavy in your stomach. Skip spicy foods, sugary foods, and sweetened beverages until you’re confident your stomach feels calm again. They can irritate your stomach lining and cause more digestive discomfort.
If you have abdominal pain or sharp cramping, pause and let your body recover again. The goal isn’t to rush. It’s to create small wins that remind you food can feel good again.
Step 3: Reintroduce Proteins and Nutrients
Once your appetite gently returns, it’s time to expand your options. You’ll want to start including lean proteins like eggs, fish, chicken breast, or tofu. These foods are less likely to trigger nausea compared to greasy or fatty foods.
A simple tip is to eat protein first in your meal. Doing this supports blood sugar control and helps stabilize blood sugar levels as your body adjusts to eating again. It also helps maintain muscle while losing weight.
You can pair your protein with non-starchy vegetables or whole grains like brown rice or oats. These add fiber and nutrients without overwhelming your digestive system. Gradually, your fiber intake will improve as you start feeling more comfortable.
Step 4: Listen to Your Stomach
Pay attention to what your body is telling you. Your stomach’s signals matter now more than ever. If you feel full quickly, don’t force another bite. Try eating smaller meals or frequent meals throughout the day. This helps minimize nausea and prevents that heavy feeling that often comes from eating too much at once.
Small, balanced plates help you stay nourished while giving your digestive system time to catch up.
Some people find that certain foods like yogurt, broth, or bananas are easy to tolerate, while others may cause mild queasiness. Keep mental notes of which foods comfort you and which don’t. This self-awareness makes it easier to manage nausea in the future.
Step 5: Add Variety Slowly
Once your nausea fades and your body adjust, you can experiment with more complex meals again. Add foods one at a time and see how you respond. Remember, your tolerance can shift daily.
Keep an eye out for high-fat, processed foods or unhealthy fats, which can affect blood sugar levels and worsen nausea. Heavy sauces, creamy desserts, and refined carbohydrates can overwhelm your digestion and trigger nausea.
Instead, focus on healthy fats like avocado, nuts, and olive oil in small amounts. These support maximum nutrition without weighing you down.
You’ll start noticing a pattern: lighter foods make you feel energized, while heavy or greasy meals might slow you down. That’s your body telling you it prefers a balanced diet that supports your diabetes management and steady blood sugar.
Step 6: Rebuild Confidence with Food
Reintroducing food after nausea is not only a physical process, it can stir up emotions as well. You may feel hesitant, worried that eating will bring discomfort again. That’s normal.
Start with foods that bring comfort, even if they’re simple. When you enjoy a small bowl of soup or a bit of rice without discomfort, that’s progress. Those moments rebuild your relationship with eating, which plays a big role in your weight loss journey.
As you continue to feel better, you can reintroduce high-fiber foods and those rich in vitamins and minerals. Gradually increasing variety helps regulate blood sugar levels and prevent weight gain.
Step 7: Pay Attention to Triggers
You’ll notice patterns in what your stomach tolerates. Some people find that spicy foods, fried foods, or high-sugar foods instantly make them queasy. Others might find large portions or eating foods too fast creates discomfort.
If you ever experience stomach pain, abdominal pain, or upset stomach, review what you last ate and how you felt after. Keeping a food journal can help identify which meals reduce nausea or exacerbate nausea.
If nausea persists, consult your healthcare provider. Occasionally, persistent gastrointestinal adverse events can signal something deeper, such as acute pancreatitis, which requires medical attention.
Step 8: Support Digestion and Comfort
As your appetite returns, think of gentle ways to support your digestive system. Start your day with water, move your body lightly after meals, and make sure to eat protein consistently.
Try to avoid high-fat foods that can cause delayed gastric emptying, making you feel bloated or nauseated again. Instead, choose simple, nutrient-rich ingredients and keep portions moderate.
You can also include a few bland foods throughout the day if you’re not yet ready for complex flavors. These help balance your food intake and calm your stomach lining.
If you notice blood pressure changes or dizziness, make sure you’re drinking enough fluids and eating small, steady meals. Semaglutide can sometimes lower blood pressure, especially if you’re eating less or losing fluids.
Step 9: Balance Comfort and Nutrition
Once your digestion feels stable, focus on achieving maximum nutrition without reintroducing too much too fast. Your plate should include a mix of protein, fiber, and healthy carbohydrates.
Think of your meals as layers: start with your protein, then add your vegetables, then finish with complex carbs. This helps with blood sugar control and supports long-term weight management.
When you eat this way, your energy feels steady and your cravings start to fade. That’s a sign your digestive system and metabolism are syncing up again.
If you still experience GI symptoms, try adjusting portion size or timing instead of cutting foods out completely. Sometimes, eating less but more often is enough to minimize nausea.
Step 10: Stay Consistent
Your progress will look different each week, but consistency matters. Once your body adjusts, you’ll notice your hunger cues become more predictable, your meals feel lighter, and you can eat a wider variety without discomfort.
That’s your body finding its balance again.
Keep sticking to frequent meals, light seasoning, and slow bites. If you ever feel queasy again, return to bland foods or easily digestible foods for a few days. It’s all part of learning to eat comfortably during treatment.
You’re not just reintroducing food, you’re rebuilding trust in your body. Each small improvement, each meal that feels good, means your system is working with you again.
When To Seek Help
Most nausea improves naturally, but if you develop intense stomach pain, prolonged vomiting, or signs of acute pancreatitis, contact your doctor immediately. While rare, these can be serious side effects.
If you find that certain foods always cause discomfort or you cannot keep meals down, your provider can help you manage gastrointestinal adverse events safely. Sometimes a change in dosage, meal timing, or an anti-nausea prescription can make all the difference.
Building Long-Term Habits
Once you’re back to regular eating, think about maintaining a healthy diet that supports your diabetes management and weight management goals. Choose whole grains, non-starchy vegetables, lean proteins, and healthy fats as your foundation.
Limit refined carbohydrates, processed foods, and meals loaded with unhealthy fats. These not only slow digestion but can also affect blood sugar levels, especially if your digestive system is still sensitive.
When you maintain this type of eating pattern, you’ll notice better energy, steadier blood sugar, and fewer digestive upsets. It’s a sustainable way to feel good while losing weight.
Small Habits That Make A Big Difference
- Eat protein with each meal to keep you full longer.
- Eat slowly and savor each bite.
- Avoid high-fat foods that sit heavily in your stomach.
- Sip water between bites instead of chugging before or after meals.
- Choose bland foods during flare-ups.
- Space out frequent meals instead of skipping.
- Include whole grains and non-starchy vegetables for natural fiber.
- Keep your fiber intake gradual if your stomach still feels sensitive.
- Rest when your stomach feels uneasy, and try light walking to help digestion.
These gentle steps make it easier to manage nausea and support your recovery while allowing your body adjusts to semaglutide treatment.
Enjoying Food Again
When you finally sit down to eat your favorite meal without discomfort, it feels like more than physical progress. It becomes a small victory that reminds you of how far you’ve come.
You’ve learned what your body likes, how to read its signals, and how to create comfort through food instead of fear. You’ve learned to listen and adapt, not to rush or restrict.
And that is how you successfully reintroduce food after nausea on semaglutide: with patience, understanding, and a renewed sense of confidence in your own body.